Enzymes (exercise in biochemistry)
|
This article was marked by its author as Under construction, but the last edit is older than 30 days. If you want to edit this page, please try to contact its author first (you fill find him in the history). Watch the discussion as well. If the author will not continue in work, remove the template Last update: Sunday, 25 Dec 2022 at 7.57 pm. |
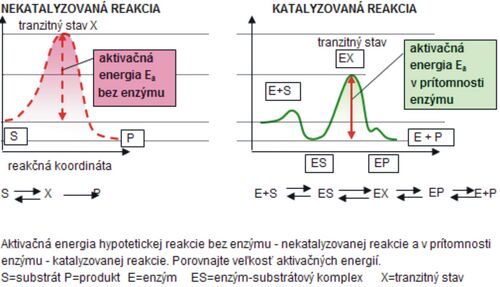
Enzymes are catalysts of biochemical processes taking place in living organisms, and therefore they are often called biocatalysts. Since they are proteinaceous substances, they are created just like other proteins by proteosynthesis, which is regulated according to the requirements of the cell and the organism. Enzymes are cleaved by proteinases and have their own biological half-life. Enzyme molecules have a defined spatial arrangement - conformation. This allows certain side chains of amino acids to get close to each other and create the so-called active site of the enzyme. The substrate (S) (substance to be converted) binds to this site, a labile intermediate product – the enzyme complex – substrate (ES) is formed, which spontaneously breaks down into the product (P) of the reaction and the enzyme (E ). Enzymes accelerate the stabilization of the chemical equilibrium of the reaction by lowering the activation energy - Ea (Fig. 1).
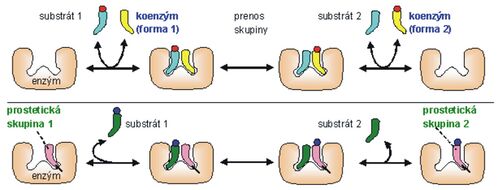
Enzymes often also contain a non-protein component, a ``prosthetic group or a ``coenzyme (Fig. 2). The protein component of the enzyme (holoenzyme) is called the apoenzyme. The coenzyme binds weakly to the apoenzyme and can dissociate from it. The prosthetic group is not released from the apoenzyme, but is firmly attached to it. Currently, the more general term cofactor is often used, which does not distinguish the binding method.
Enzyme' (holoenzyme) = apoenzyme + cofactor (prosthetic group, coenzyme)
Division and catalytic activity of enzymes[edit | edit source]
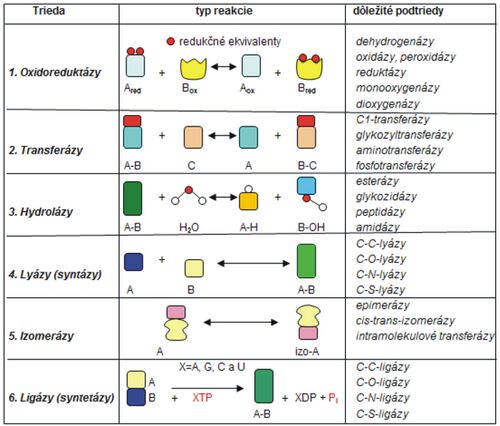
The following table (tab. 1) clearly lists the individual classes of enzymes and schematically shows their effects (the type of reaction that individual enzymes catalyze). Examples of several specific cofactors are also listed in the table.
Expression of enzyme activity[edit | edit source]
Enzyme activities are expressed in units according to the international system of units (Systeme International d'Unides - SI) and the recommendations of the IFCC (International Federation of C'linical 'Chemistry). The unit for expressing enzyme activity in the SI system is the "catal" (cat), which is most often used in conversion to 1 liter of biological fluid.
Definition: 1 cat is the enzyme activity that converts 1 mol of substrate in 1 s.
In professional biochemical as well as medical practice, we still encounter the international unit U, which was officially used until 1980. The international unit U was defined as the activity of an enzyme that converts 1 µmol of substrate in 1 min at 25 °C. Since it is still used, we present the basic mutual conversion of these units:
1 cat' = 1 mol · s−1 = 60 mol · min−1 = 60.106 mmol · min−1 = 6.107 U
Kinetics of enzyme reactions[edit | edit source]
The Michaelis constant (Km) is defined as the substrate concentration at which the rate of the enzyme-catalyzed reaction is halved. Km is a basic kinetic constant that is characteristic for each enzyme-substrate pair under the given conditions (pH, temperature, composition of the reaction mixture, etc.). It is expressed by the relationship of the modified Michaelis-Menten equation:
Determination of Km[edit | edit source]
Km we can determine (Fig. 3):
- from a graphical representation of the dependence of the reaction rate on the concentration of the substrate, while it is difficult to determine the maximum rate with sufficient accuracy
- by modifying the Michaelis-Menten equation, in which the hyperbolic dependence is transformed into a linear one, we obtain a more accurate relationship for the calculation of Km. The most common is the adjustment according to Lineweaver and Burke, in which the inverted values of the speed and concentration of the substrate are evaluated.
(Vmax – maximum speed, Km – Michaelis constant – assumption is that [E] = const.)
Types of enzyme activity inhibition[edit | edit source]
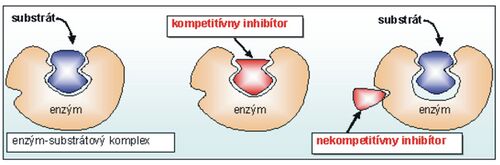
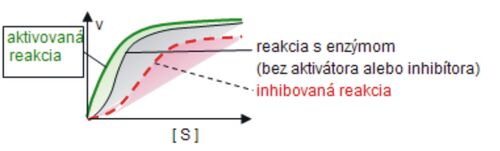
Enzymes are characterized by high specificity towards the substrate (substrate specificity) and the type of catalyzed reaction (effect specificity). Their activity can change rapidly depending on the needs of the cell and the whole organism. 'Activators stimulate and inhibitors inhibit the rate of enzyme reactions. Inhibition can be reversible or irreversible. In contrast to irreversible inhibition, reversible inhibition involves non-covalent binding of the inhibitor, whereby we distinguish competitive, non-competitive and acompetitive inhibition. Figure 4 shows the distinction between a competitive and a non-competitive inhibitor.
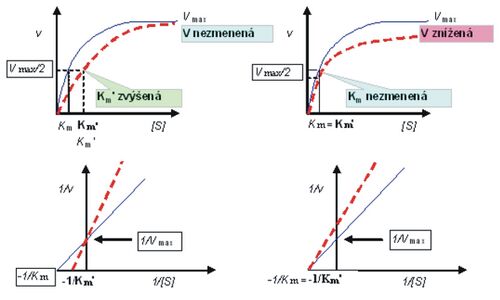
The following figure (Fig. 5) shows the influence of substrate concentration (S) on the rate (v) of the enzyme reaction depending on the inhibitor and the dependence of Km on the type of inhibition:
(blue line without inhibitor, red with inhibitor – competitive on the left and non-competitive on the right)
Factors affecting the rate of an enzyme reaction[edit | edit source]
In a living cell, enzymes are arranged in such a way that the individual reactions smoothly follow each other, so they often create so-called multienzyme complexes. Compared to inorganic catalysts, enzymes are much more effective, but also more sensitive to external influences (temperature, pH, etc.). Enzyme-catalyzed reactions take place in a living organism (even in a test tube) at a different rate, which depends on:
- substrate concentration
- enzyme concentration
- temperatures
- reaction medium (pH)
- the presence of activators and inhibitors
Substrate concentration[edit | edit source]
The concentration of the substrate at which the reaction rate of the enzyme-catalyzed reaction corresponds to half the value of the maximum rate is called the Michaelis constant - Km of the enzyme of the given reaction (Fig. 3).
Enzyme concentration[edit | edit source]
For the speed of the enzyme reaction at high substrate concentrations, the following applies:
Vmax = k · [E]T = const.
All experiments to determine the effect of enzyme concentration on the reaction rate must be done with an excess of substrate, when the reaction is no longer dependent on the effect of its concentration.
Effect of temperature on enzyme activity[edit | edit source]
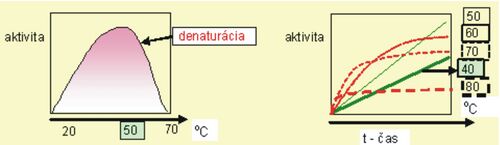
Another important factor that affects the catalytic activity of the enzyme is ``temperature (Fig. 6). As the temperature increases, the activity of the enzymes (in the range from 20-50 °C) increases approximately twice. At higher temperatures, the speed of the reaction gradually decreases, because the enzymes denature (with exceptions – e.g. enzymes of thermostable bacteria). The temperature at which the enzyme exhibits maximum activity is called the enzyme's temperature optimum. For most enzymes, the temperature optimum is in the range of 35–45 °C. At temperatures around the freezing point, reactions hardly take place. Deep freezing at −20 °C is used to preserve biological material, when enzyme reactions are completely stopped.
Effect of pH on enzyme activity[edit | edit source]
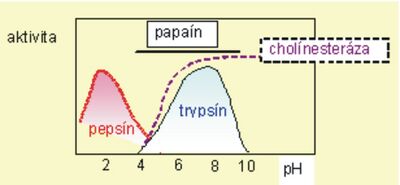
One of the factors that significantly affects enzyme activity is the pH value of the environment. The use of strongly acidic or strongly alkaline solutions can even cause denaturation of the enzyme and thereby loss of biological properties. Less drastic changes in the pH of the environment affect the activity by changing the degree of dissociation of functional groups of the enzyme and the substrate, or by changing the conformation of the enzyme molecule. This will change the ability of the substrate to bind to the enzyme. Most enzymes show maximum activity in the range of pH values 5–8, and this region is known as the optimum pH. Of course, there are exceptions and some enzymes have pH-optimums at significantly different values, e.g. for pepsin it is pH 1.5–2.5 or for alkaline phosphatase 9.5–9.7. The graphically expressed dependence of the reaction rate on pH usually has the shape of a bell-shaped curve with a peak at the optimal pH (Fig. 7).
The catalytic activity of the enzyme is also affected by the change in the ionic strength of the solution and the composition of the buffer, redox conditions, ionizing radiation or the addition of inhibitors or activators.
Enzymes in clinical diagnostics[edit | edit source]
Enzymes in cells influence biological processes by participating in the regulation of metabolic and functional processes. Damage to cells can lead to changes in enzyme activities, and enzymes can be released into the blood after cell damage. From the point of view of the biochemical methods themselves, it is necessary to evaluate the dynamics of the detected changes in the patient and it is not possible to rely only on the assessment of one investigated parameter.
Enzyme isoforms[edit | edit source]
Determination of isoenzymes is important for increasing diagnostic specificity. We distinguish between true isoenzymes, which are encoded by different structural genes, and pseudoisoenzymes, which have the same genetic basis, but differ in post-translational modifications (post-translational variants, e.g. ALP – pseudoisoenzymes of bile ducts, tumor cells) . True isoenzymes are formed:
- by modifying genes in different loci (the same in all humans, they arose in the course of evolution), e.g. isoenzymes AST – mitochondrial, cytoplasmic or ALP – intestinal, non-tissue-specific (liver, bone, kidney), placental, fetal;
- by modifying genes in the same locus, different alleles (congenital gene variations), for example glucose-6-P-dehydrogenase was isolated from erythrocytes of different people in more than 150 isoforms;
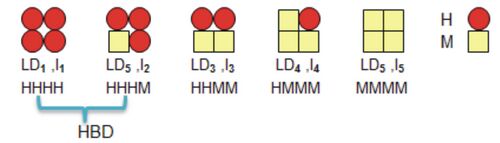
- as so-called hybrid isoenzymes by combining at least 2 subunits encoded by different structural genes, e.g. lactate dehydrogenase (LD, Fig. 8) containing subunits H (heart) and L (muscle) or creatine kinase (CK, Fig. 9) composed of subunits B ( brain) and M (muscle).
Use of isozyme determination in serum'
Isoenzymes catalyze the same reaction, but their molecules differ in their physicochemical, kinetic and immunological properties. These differences can be manifested, for example, in the relationship of isoenzymes to inhibitors, in the specificity of catalyzed reactions, in different resistance to denaturing influences, have different pH optima and differ in the protein component.
Enzymes in the blood[edit | edit source]
The determination of enzyme activities in the serum is, together with other methods of clinical biochemistry, one of the important examinations that help the doctor determine or confirm the diagnosis and inform about the course of the disease. In order to correctly interpret the values of enzyme activities, it is necessary to know the factors that influence their activity in the serum and that also determine the appropriateness of examining certain enzymes during the course of the disease.
Factors affecting the activity of enzymes in the blood[edit | edit source]
Origin and Role of Enzymes
Enzymes found in plasma can be divided into ``secreted and ``cellular. Secretory enzymes are released into the environment and can be divided into:
- functional plasma enzymes - their role is to catalyze reactions taking place in the bloodstream. These include, for example, enzyme complexes involved in blood clotting. Some of these enzymes are produced in the liver and therefore their activity in the plasma decreases when it is damaged.
- functional GIT enzymes (specific) - they catalyze the reactions taking place in the GIT and thus enable the digestion and absorption of the components of the food received. This group includes, for example, pancreatic enzymes (eg amylase, lipase, trypsin). If there is an obstacle in the ways by which these enzymes reach the alimentary canal, or if there is more damage to the cells in which they are formed, the activity of these enzymes in the serum increases.
Cellular enzymes represent a large group of enzymes that play a role in cell metabolism and enter the bloodstream when they break down or are damaged. Their activity in the serum rises significantly when the organs from which they originate are damaged. These include, for example, tranaminases, creatine kinase, glutamate dehydrogenase. A small part of these enzymes is released into the bloodstream even under physiological conditions.
'Activities of individual enzymes in cells The specific tasks of organs and cells are closely related to their metabolism. Therefore, different organs and cells also contain different amounts of enzymes (table 2). The different activities of enzymes in the organs are among the main factors on which the change in their activities in the serum also depends. Due to the constant remodeling of organs, we can prove their activity in the serum even under physiological conditions.
Tab. 2 Activities of selected enzymes
| Enzyme | Liver | Heart | Skeletal muscle | Erythrocytes | Serum |
|---|---|---|---|---|---|
| nkat.g-1 | nkat.ml-1 | ||||
| AST | 980 | 870 | 600 | 13.34 | 0.4 |
| ALT | 580 | 48 | 57 | 1.7 | 0.4 |
| LD | 2,420 | 2,068 | 2,450 | 600 | 4 |
| CK | 12 | 5,830 | 33,840 | < 0.1 | 0.83 |
| GMD | 630 | 18 | 8 | < 0.1 | 0.06 |
| Aldolase | 95 | 82 | 800 | 16.7 | 0.07 |
Another factor that influences the level of enzymes in the blood is the rate of enzyme release into the serum, which can be influenced primarily by the binding of the enzyme to cell particles, the physicochemical properties of the enzyme molecule and the localization of the enzyme in the cell. When the cell membrane is damaged, enzymes located in the cytoplasm can be released into the environment earlier than, for example, enzymes bound in mitochondria. Enzymes enter the bloodstream not only during the breakdown of a cell, but also after it has been damaged, e.g. by a lack of oxygen or by harmful substances. These processes can increase the permeability of the cell membrane and under these conditions the size, charge and shape of the protein molecule of the enzyme as well as its localization play an important role.
Decisive factors that affect the level of enzyme activity in the serum and the duration of its rise after release into the blood include the ``inactivation and elimination of enzymes. Both factors depend on the properties of the enzyme molecules and the systems that eliminate the enzymes. To express the decrease in enzyme activity in the serum, we use the rate of inactivation or elimination as an indicator - the biological half-life of the enzyme''''(t1/2), which expresses how long the activity of the enzyme drops to half its value. The biological half-life is one of the factors that directly affect the diagnostic use of individual enzymes (suitability of their examination during the course of the disease). The following table lists selected elimination half-lives of some important enzymes in serum.
| Enzyme | t1/2 | Enzyme | t1/2 |
|---|---|---|---|
| amylase | 3–6 h | ALT | 47 h |
| lipase | 3–6 h | LD1 | 113 h |
| LD5 | 10 h | HBD | 113 h |
| CK | 3pm | GMT | 3-4 days |
| AST | 17 h | ALP | 3-7 days |
| GMD | 18 h | CHS | 10 days |
The ``character of the disease process also has a significant influence on the activity of enzymes in the blood. The phase and extent of tissue damage by the disease process also determines the amount of enzymes released from the cells into the plasma. This process can be influenced by the degree of vascular supply at the site of pathological changes, the speed of circulation in this area and the presence/absence of an inflammatory barrier that separates the damaged part of the tissue from the surroundings.
When interpreting increased levels of enzymes in the serum, it is important to assess other factors such as age, gender, physical activity, fluid balance, medications, alcohol, but also interference from the point of view of organ changes, or interference from methodological reasons - the so-called '' non-specific influencing of enzyme activity.
Diagnostically significant enzymes[edit | edit source]
The following table lists selected clinically important enzymes.
| Enzyme (abbreviation) | Increased values | Decreased values |
|---|---|---|
| Alanine aminotransferase (ALT) | various liver diseases | |
| Alkaline phosphatase (ALP) | physiological during growth and pregnancy, diseases of the liver and biliary tract, bone diseases, convalescence after fractures, some tumors | reduced thyroid function, Wilson's disease, zinc deficiency |
| Amylase (AMS) | inflammation of the pancreas, gl. parotid inflammation, various diseases of organs in the abdominal cavity | |
| Aspartate aminotransferase (AST) | liver disease, striated muscle damage, heart muscle damage | liver failure |
| Elastase | pancreatic diseases | |
| 3-hydroxybutyrate dehydrogenase (HBDH) | monitoring of the course of myocardial infarction | |
| Glutamyltransferase (GMT) | biliary tract and liver disease (especially toxic damage – drugs, alcohol) | |
| Cholinesterase (CHS) | liver diseases, organophosphate intoxication, hypercatabolism | |
| Creatine kinase (CK) | myocardial infarction (CK-MB), skeletal muscle diseases, intramuscular injections, physical activity (CK-MM), brain diseases, some tumors (CK-BB) | |
| Acid phosphatase (ACP) | overproduction of parathyroid hormone, prostate tumors, bone tumors | |
| Lactate dehydrogenase (LD) | myocardial infarction, anemia (LD1,2), pulmonary embolism (LD3), liver disease, skeletal muscle disease (LD4,5), tumors (LD3–5) | |
| Lipase (LPS) | pancreatitis | |
| Trypsin | pancreatic disease | juvenile diabetes, cystic fibrosis |
| Thymidine kinase | tumors, viral infections | |
| Most coagulation factors | coagulation disorders | coagulation disorders |
Distribution of diagnostically significant enzymes in tissues[edit | edit source]
The following table shows the distribution of selected clinically significant enzymes.
| Enzyme | ACP | ALP | AMS | ALT | AST | CK | GMT | CHS | LD | LPS | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Erythrocytes | ** | * | * | ||||||||||
| Bones | * | ** | |||||||||||
| Skeletal Muscle | * | * | ** | * | |||||||||
| Myocardium | * | ** | * | ||||||||||
| Kidneys | * | * | * | * | |||||||||
| Pancreas | ** | * | ** | *** | |||||||||
| Liver | * | * | *** | *** | * | ||||||||
| Prostate | *** | ||||||||||||
| Biliary tract |
LD is an example of an enzyme that occurs not only in tissues capable of anaerobic metabolism (erythrocytes, muscles), but also in organs where lactate oxidation via pyruvate and acetylCoA (heart, neurons) or gluconeogenesis (liver) occurs. An increased level of LD in plasma may indicate damage to such an organ, which we can use in diagnostics. Serum CK originates 96% from skeletal muscle and 4% from myocardium. When skeletal muscle is damaged, the overall activity of CK increases. When a myocardial infarction is suspected, it is important to rule out skeletal muscle damage.

![{\displaystyle K_{m}=[S]\cdot [{\frac {V_{max}}{V-1}}]}](https://wikimedia.org/api/rest_v1/media/math/render/svg/058d1ccfd1bc1c9855369d0e0978eb1d4ebe7b5c)
![Fig. 3 Saturation curve - effect of substrate concentration [S] on enzyme reaction rate](/thumb.php?f=StanovenieKM.jpg&width=500)