Editing Tuberculosis (pneumology)
From WikiLectures
Tuberculosis (TB) are all disease states caused by the Mycobacterium tuberculosis complex.
Epidemiology[edit | edit source]
- Tuberculosis is a specific infectious disease, occurring in both ancient Greece and the Roman Empire.
- It is currently the most common deadly infectious disease in the world, with about 20 million people suffering from tuberculosis and about 3 million people dying from it every year.
- Tuberculosis remains a social disease.
- The most common source of tuberculosis is a person with tuberculosis.
- The term tuberculosis was introduced in 1834 by Scholein, but the etiology of tuberculosis was clarified by Robert Koch.
Etiology[edit | edit source]
- Human tuberculosis is caused by Mycobacterium tuberculosis, Mycobacterium bovis and Mycobacterium africanum - collectively referred to as Mycobacterium tuberculosis complex.
- Mycobacterium tuberculosis is an acid-resistant, alkali-resistant and alcohol-resistant aerobic microbe with optimal growth at a temperature of 37–38 ° C and a long generation time, which requires cultivation on special soils for 12 weeks.
Pathogenesis[edit | edit source]
- Transmission is by inhalation (droplet). Transmission is also possible by direct contact (inoculation) and food.
- The gateway to the infection is 80-90% of the respiratory system.
Division[edit | edit source]
- Primary tuberculosis - occurs after the first contact with a mycobacterial infection. Under suitable conditions, mycobacterium tuberculosis enters the lungs, where it multiplies and causes a local exudative inflammatory reaction - the primary infection. Within a few hours, Mycobacterium tuberculosis spreads through the lymphatic system to regional nodes, which enlarge and together with inflammation in the lungs form a primary tuberculosis complex.
- Primary tuberculosis from TB lymphadenitis often spreads, the "syrupy" node perforates the bronchus and gives rise to aspiration spread of tuberculosis.
- In 90% of cases, they heal spontaneously with the development of hypersensitivity to tuberculin.
- Post-primary tuberculosis - in people already infected and most often affects the lungs.
- A common form of post-primary tuberculosis is the early Asmann-Redekeru subclavian infiltrate.
- After a certain time, the infiltrate succumbs to caseous necrosis → spread of tuberculosis by aspiration.
- It also spreads either directly to the surroundings, by coughing up and swallowing sputum (tuberculous laryngitis, intestinal tuberculosis), lymphatic vessels or hematogenously.
- Exogenous infection (reinfection 30%) - inhalation of new mycobacteria in contact with the patient.
- Endogenous reactivation by primary tuberculosis when weakened by malnutrition, pregnancy, alcoholism.
- Healing of lesions by post-primary tuberculosis is associated with collagen ligament proliferation, scarring and fibrosis of the lung parenchyma.
Clinical picture[edit | edit source]
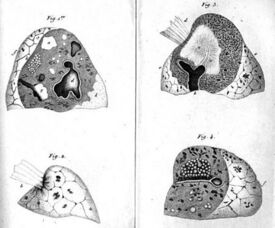
Pathological formations arising from pulmonary tuberculosis
- The primary infection can be asymptomatic, rarely in children with higher temperatures, anorexia, decreased activity.
- Post-primary tuberculosis can also occur asymptomatically or with creeping characteristic problems under the influence of influenza.
- The functional symptoms of most TB manifest as marked fatigue, anorexia,weight loss, decreased physical performance, subfebrile, night sweats, dry, later productive cough, mucoid to mucopurulent sputum.
- It is an alarming symptom hemoptysis.
Diagnosis[edit | edit source]
- Isolation Mycobacterium tuberculosis from various materials (in lung diseases, sputum, aspirate obtained by bronchoalveolar lavage, gastric aspirate and occasionally laryngeal swabs of people who do not cough are examined).
- Microscopic examination after special staining (Ziehl-Neelsen),it is possible to demonstrate acid-resistant rods within 24 hours.
- Culture tests on various media are evaluated at the earliest after 3, then after 6 and 9 weeks, the negative result is when Mycobacterium does not grow on the media even after 12 weeks.
- Polymerase chain reaction - PCR.
- RTG –bearing shadows in the upper thirds of the lung fields, can be seen clearing the cavern.
- Mantoux II test positive (greater than 6 mm in 72 h), after intradermal application of 2 tuberculin units.
- QuantiFERON
Severe forms of tuberculosis[edit | edit source]
- Million TB
- Induced by hematogenous spread of mycobacteria and all organs (lungs, liver, meninges, spleen) are affected.
- The clinical picture is changeable. We distinguish three forms of the disease:
- typhoid form – suddenly formed septic conditionv s tachycardia, unresponsive to common antibiotics;
- pneumonic form – stuffiness,cyanosis, tachycardia, tachypnoea;
- meningitic form - obesity, slow speech, headache, meningeal symptoms.
- Diagnosis - chest X-ray - symmetrical distribution of the shadow of miliary deposits (1 mm in diameter).
- Tuberculous pneumonia
- It suddenly begins with chills, chills, fever, profuse sweats, congestion, cough with purulent expectoration.
- The creation of a cavern leads to a correct diagnosis, no antibiotic effect and cultivation distinguishes from bacterial pneumonia.
Diagnosis of tuberculosis[edit | edit source]
- It is determined on the basis of symptoms, a characteristic finding on the chest skiagram and evidence of mycobacteria.
- Differential diagnosis: all non-specific lung diseases should be considered pneumonia, bronchogenic carcinoma, sarcoidosis,pulmonary infarction, silicosis, Wegener's granulomatosis, …
Therapy[edit | edit source]
- Susceptibility to antituberculotics
- Primary resistance –a drug-resistant strain in an otherwise usually sensitive mycobacterial species obtained from a patient who has demonstrably never been treated with this drug (1-2% in the Czech Republic).
- Initial resistance is a combination of primary resistance and undetected acquired resistance if previous use cannot be ruled out or demonstrated antituberculotics.
- Acquired (secondary) resistance –the initially sensitive Mycobacterium strain became resistant to the drug that the patient had been taking for more than one month during or after treatment. It is usually the result of incorrect treatment.
- Polyresistence (MDR)is a condition in which tuberculous mycobacteria are resistant to multiple antituberculotics, at least isoniazid and rifampicin. It is the most severe form of bacterial resistance that results from the misuse of drug regimens.
- Antituberculotics
- Bactericidal - kill dividing bacteria (nidrazide, rifampicin, streptomycin).
- Sterilizing effect - they kill the so-called "persistors" (pyrazinamide, rifampicin).
- Bacteriostatic antituberculosis drugs (ethambutol).
- Rifampicin (RMP, R)
- The most effective bactericidal antibiotic, administered orally in the morning on an empty stomach in a dose of 450-600 mg.
- It acts on Mycobacterium with low metabolic activity.
- It turns orange with saliva, sweat, urine.
- Side effects: hepatitis, trombocytopenia with purple, flu problems („flu-like“ syndrom), allergies, kidney damage and indigestion.
- Isoniazid (isonicotinic acid hydrazide, INH, H)
- It is administered orally at a dose of 5 mg / kg body weight on a daily basis.
- An effective and inexpensive bactericidal drug with effect on extra - and intracellular Mycobacterium.
- It is given preventively after contact with TB.
- Side effects: peripheral neuritis, hepatotoxicity and allergies.
- Streptomycin (STM, S)
- It is an aminoglycoside antibiotic, administered intramuscularly 0.75-1.0 g once a day.
- It has a bactericidal effect on extracellularly deposited mycobacteria.
- Side effects: ototoxicity and nephrotoxicity, allergic skin reactions.
- Pyrazinamide (PZA, Z)
- It is administered orally at a dose of 1.5-2.0 g / day.
- It has a bactericidal effect on intracellular phagocytosed mycobacteria.
- It is hepatotoxic and affects the tubular secretion of uric acid (hyperuricemia, dna).
- Ethambutol (EMB, E)
- It is administered orally at a dose of 25 mg / kg body weight.
- Synthetically prepared antituberculotics with mycobacteriostatic effect.
- A serious side effect is the development of retrobulbar neuritis with visual disturbances and color vision.
Principles of treatment[edit | edit source]
- Combined, long-lasting and controlled to prevent resistance.
- In combination with at least 3 drugs in a single morning dose under the control of the nursing staff.
- Institutional treatment (initial phase) is usually limited to 2 months, eg 2 HRDs, when infectivity is reduced to a minimum and possible drug interactions and side effects of initiated therapy are assessed. We perform further treatment (continuing phase) on an outpatient basis daily, eg 4 RH - 4 months RH, or intermittently, eg 4 R3H3 - 4 months 3 times a week RH.
- The minimum duration of treatment with bacteriologically confirmed TB is 6 months, unverified 4 months.
- Dispensary care (a set of measures that includes preventive methods, search and reporting, proper treatment, continuous monitoring of health status and maintenance of working capacity).
Links[edit | edit source]
[edit | edit source]
External links[edit | edit source]
- Tuberculosis on stefajir.cz
- Tuberculosis of bones and joints - Review article of the radiodiagnostics report, volume 51, No. 1/2005
- Tuberculosis and respiratory diseases (ÚZIS ČR)
References[edit | edit source]
HOMOLKA, Jiri, et al. Internal Medicine Volume III. first edition. Praha: nakladatelství Galen, 2001. 122 pp. 60 - 71. https://www.wikiskripta.eu/w/Speci%C3%A1ln%C3%AD:Zdroje_knih/80-7262-131-9