ELECTRO THERAPY
7.3. ELECTRO THERAPY[edit | edit source]
Electrotherapy is commonly used for physical therapy (PT). When correctly indicated and applied it is very effective. However, it cannot be lifted out of the context of comprehensive therapy, neither regarded as a cure-all. Most of the physical procedures have similar effects and depending on the parameters, some of them may be dominant. The main effects are: analgesic, myorelaxation, trophic and anti edematous.
7.3.1. CLASSIFICATION OF ELECTROTHERAPEUTIC CURRENTS[edit | edit source]
Electric currents used in therapy are conventionally divided into three basic groups: galvanic current, pulse direct current and alternating current.
Galvanic Current Galvanic current (or “continuous”) is a current of constant intensity. It is always DC. It is used mostly for iontophoresis, or its trophic stimulation (hyperemic) effect is utilized. A big disadvantage of the galvanic current, is the risk of chemical damage of the tissue under the electrodes. The damage may be caused by the hydrochloric acid which originates under the anode or by the soda layer that originates under the cathode. Similar types of tissue damage can occur also at any direct current (e.g. diadynamic). Direct currents must not be used on patients with metallic implants! At present this current is often substituted by galvanic intermittent current. This current has the same effects (galvanic component is 95 %) but due to interruption of the originally continuous intensity by the frequency of 8 kHz it is better tolerated by the patients. It is suitable especially for iontophoresis.
Pulse Direct Current The pulse direct current is of variable intensity but only one polarity. The basic pulse shape may vary. It includes e.g. diadynamics (combination of pulse DC – “dosis” and galvanic current – “basis”), rectangular (e.g. Träbert current), triangular and exponential pulses of one polarity. Depending on the used frequency and intensity it has stimulatory, trophic and analgesic effects. Generally, direct currents with variable intensity implies the same risks as galvanic current (corrosion of the skin surface) and therefore it requires careful observation of the procedure. Note the correlation between the applied intensity and the length of application. The main effect is stimulation which is important, especially below the cathode (green negative electrode).
Alternating Current
In comparison with DC, alternating current is safer and better subjectively tolerated by the patient. The basic pulse shape again may vary – rectangular, triangular, and harmonic sinusoidal, exponential or combined. It can be alternating, symmetric or asymmetric. The DC component is always zero, which prevents chemical damage of the skin under the electrodes.
Therefore, this current allows also for long-lasting applications. It can even be used on patients with metal implants. Note that Implanted electronic stimulators such as pacemakers etc. are indeed absolute contraindications for applying AC Electrotherapy. Use of alternating currents in contact electrotherapy implies much lower stress on the tissue under the electrode. For these types of currents the capacitive component of skin resistance is involved, and due to that these currents are very well tolerated by the patients.
In general: • short duration of the pulse improves the subjective perception, • the zero average value (DC component) prevents chemical damage of the tissue, • frequency and amplitude are responsible for the required therapeutic effect.
There are 5 subtypes of alternating currents used in therapy: TENS, Classic (four-pole) Interference, Two-pole Interference, Isoplanar Interference and Dipole Vector Field.
1) TENS (transcutaneous electrical nerve stimulation) It is a group of prevalent currents substituting the standard applications of diadynamic currents. They are low-power and have zero DC components. Therefore, besides suppression of chemical damage of the tissue, the risk of electric damage of the tissue is also minimized. As can be derived from their names, these currents are intended for stimulation of nerve roots or nerve fibres. Their major utilization is alleviation of pain, inhibition of itching, etc. The mechanism of their effect is most often explained by the so-called gate theory of pain. Besides treating pain, these currents can also be effectively utilized in electro-gymnastics (stimulation of denervated muscles).
2) Classic (four-pole) Interference Four electrodes are located crosswise. Two frequency signals with different frequencies fA and fB are brought to the tissue. Their interference in the tissue induces a low-frequency surge in the centre of the cross; its frequency is: AMF = fA - fB. This surge of the frequency AMF has therapeutic effect; both basic currents of the frequency fA and fB are used only for "transport" of the AMF surges to the tissue. The fA frequency is constant; changes of the fB frequency by the value of so-called Spectrum serve for change of the resulting frequency AMF to the frequency AMF + Spectrum. Interference has similar effects as the low-frequency currents although, it is carried by currents of higher frequencies and does not stress the tissue under the electrode so much. The carrier frequency of channels ranges from 3.5 to 10 kHz. The higher this frequency is, the better it is tolerated by the patient. The advantage of the four-pole interference is the in-depth aiming of the treated area and lower stress on the superficial skin. Therefore there can be set higher intensity values than for the two-pole application.
3) Two-pole Interference According to the new recommended terminology, these groups should be called "bipolar-applied amplitude-modulated mid-frequency currents"; however, owing to the length of this name we are keeping to the original one. The resulting low-frequency current of the frequency AMF (or AMF + Spectrum) is created by the equipment. Therefore two electrodes are sufficient for its application. The absolute intensity values that can be reached are lower than for the classic interference (this current is lesser tolerated by the patient than the classic interference) and at the same time the stress on the skin surface is higher than for the classic interference. Its advantage is that it can be applied by the point electrode and thus it can be effectively used in combination with therapeutic ultrasound.
4) Isoplanar Interference
It is a special form of the four-pole interference, where the additional modulation of both channels enables to distribute the current circuits to the whole space of treated area. It implies that the placing of individual electrodes is much easier – i.e. they do not need to form a perfect cross anymore. The effect of these currents are very diffuse, in-depth and delicate.
5) Dipole Vector Field Additional phase and amplitude modulation of basic signals of the four-pole interference, enables achieving only one direction of the electric field’s acting (so-called dipole is created in the tissue). In the direction of this dipole, the modulation of the field reaches up to 100 %, in the other directions it is almost zero. You can either rotate this dipole (abscissa) manually, and thus precisely aim the required effect of the therapy at the treated tissue, or let it rotate automatically.
7.3.2. EFFECTS OF ELECTROTHERAPY[edit | edit source]
Analgesic effects
Pain is a multi-factor phenomenon and studies shows that various types of pain respond variably to several physiotherapeutic, i.e. also electrotherapeutic procedures. There are several mechanisms through which the analgesic effect of electrotherapy is achieved – besides the well-known gate theory of pain there is also proven increase of production of endogenous opioids. The analgesic effect is also supported by the trophic effects of the flowing current.
With time, myorelaxation removes the muscular hyper-tone and thus also pain of myofascial origin. Since the analgesic effect of electrotherapy is fundamental and common in practice, it shall be described in a little more detail. Pain is usually simply defined as an unpleasant sense and emotional experience, connected with actual or potential damage of the tissue. We usually distinguish between acute and chronic pain. Acute pain is short-lasting (maximum several days or weeks). It is caused by mechanical damage of the tissue or by a disease, comes immediately after the painful stimulus and subsides after its ending. The intensity of acute pain depends on the intensity of stimulation. On the other hand, chronic pain is long-lasting (more than 3 months) or recurrent. Its intensity does not depend on the intensity of stimulation; emotions particularly play a leading role. Now, the general accepted theory of pain perception is based on the assumption that the existence of a specific sensory system, which transfers information from receptors of pain (nociceptors) to the central nervous system by preformed special neural pathways. However, the process is in fact much more complicated and persons interested can learn about it from the available specialized literature.
To understand the effects of electrotherapy it is important to understand especially the modulating factors influencing the perception and transfer of the painful stimulus: • The first crucial modulation factor is described by the so-called gate theory of pain. It is based on the presumption that; the nervous mechanism in the posterior medullary horns acts like small gates which only passes through a limited amount of nerve impulses from the peripheral afferent fibers to the central nervous system, depending on how much it is opened. Stimulation of some particular fibers can modulate the extent of the gates opening or closing for pain, and thus also increase or decrease transfer of the nociceptive information. A similar gate system is supposed to exist also on the level of Thalamus. • The other important modulation factor is described by the neuromodulation theory which is based on the analgesic effect of some substances belonging to the group of so-called neuromodulators. Especially endorphins and enkephalins. These substances are produced in the central nervous system and according to the mentioned theory, they have crucial importance especially for subjective perception of pain. Anyways, the analgesic effect of electrotherapy is used most often. To make PT beneficial for the patient, it is necessary to consider the following principles: • Do not suppress the signaling and protective function of pain (which is important for acute pain!), i.e. at first decrypt the information being signalized by the pain. Then properly determine the diagnosis or at least a preliminary hypothesis, and only then intervene against the pain. Pain modified by PT or analgesics can lose its specificity in so much that it later cannot be decrypted. • Together with application of analgesic PT it is necessary to consider a reduction in the administration of analgesics. This rule is very important. Owing to the possibility of relatively precise determination of the analgesic effect of PT (in contrast to the unnamed effect of medicaments), and possible undesired interaction between PT and the medicaments. • When choosing the type of PT consider the expected effect (gate theory, endorphins). • For chronic or recurrent complaints do not obstinately apply various types of PT, but examine the locomotive system (or get it examined by a specialist). Very often, the source of these complaints is far from the place of projection of pain (catenation-generalization).
For stimulation of thick, myelinated nerve fibers of A beta and delta types (gate theory), it is suitable to use low frequency currents of the frequency 50 - 150 Hz (optimum 100 Hz) and intensity at or above threshold sensitivity. This method is effective especially for acute and segmentally localized pain. For chronic painful syndromes it is most suitable to use low frequencies 2 - 8 Hz, and intensity at the highest tolerable level (up to the threshold of pain); thus thin fibers of C type are stimulated (creation of endorphins). For achievement of both above-stated mechanisms in combination to ease the pain use the "burst modulation". The carrier frequency should be about 100 Hz, burst frequency up to 10 Hz (even frequencies lower than 1 Hz are not exceptional). Currents with burst modulation bring the cumulated analgesic effect. By the depth of the required effect the procedures can be ordered as followed: • analgesic effect of an electro tonus (galvanic current) • diadynamic currents LP and CP-ISO • Träbert current
TENS • 2-pole interference (amplitude-modulated mid-frequency currents), • 4-pole interference, isoplanar interference and vector fields
Myorelaxation and spasmolytic effect
Especially after posturographic examination have proved that overall administering of so-called myorelaxants has a negative long-term influence on the body posture. The possibility of precisely targeting the hypertonic muscle has been regarded as an especially valuable advantage of myorelaxation procedures. Overall application of myorelaxants first affect the phasic muscles which have been already weakened due to the layer syndrome. Only later, or when a stronger dose is applied, will the tonic muscles also be affected. This effect lasts for several weeks and affects the static of the spine very negatively even after the acute complaints have subsided. Procedures with myorelaxative effect include therapeutic ultrasound, 2-pole interference with contour frequency 100 – 200 Hz, 4-pole interference currents and high-voltage therapy in the same frequency modulation band. For small superficial muscles especially on hands, paraffin can also be used. A favourable side effect of myorelaxation is also the analgesic effect.
Trophic effect
Trophic effect is caused by hyperemia. It occurs in almost all types of PT (except cryotherapy). Since the mechanism of hyperemia in various types of PT is different, it is necessary to take these mechanisms into account to be able to select a suitable PT. Generally, galvanization can be recommended. Especially longitudinal (capillary hyperemia, vessel eutonization), low-frequency currents of the frequency 30 - 60 Hz and the intensity at or above the threshold motor activity level (muscle micro-pump) or ultrasound, laser, polarized specified achromatic light, vacuum-overpressure therapy, etc. The trophic effect may be partly caused by the fact that most forms of PT, esp. laser, biolamp and magnetotherapy, bring energy into the organism and is used by cells (or other structures) for their activity. The trophic hyperemic effect is also usually connected with the analgesic effect.
Anti-edematous effect
is practically connected with hyperemia, vessel eutonisation and higher capillary permeability. Therefore the therapies referred to as trophic are also anti-edematous (see the previous paragraph).
Placebo effect
Opponents of physical therapy tend to refer to its effects as placebo. If PT is applied accidentally without knowledge of its mechanism, accurate aiming and dosage (as it often happens), its effects are known as placebo. Exact verification of the effects of PT faces many troubles. • Owing to the fact that lege artis application of PT requires to take into account especially the patient's individuality and momentary functional status (including the limbic system status, mood, muscular tonus, season of the year, weather, motivation, attitude to the troubles, etc.) it is almost impossible to create a group for further statistical processing. Creation of a control group is practically out of question. • The effect of PT lies almost only in affecting the afferent system. The afferent system processes all data including the visual, auditory, tactile and other analysing impulses. Since a slight stimulus very often is sufficient to deviate the organism from the existing functional balance (even a pathological one), and using its enormous self reparation abilities, the organism helps itself. This is why there cannot be carried out e.g. a blind experiment without at least a minimum of excitation of an afferent system and/or higher components of CNS. • Functional defects of the locomotive organs which belong to the main positive effects of PT tend to self-repair if they are not prevented from it (e.g. by inappropriate pharmacotherapy). If correctly indicated, PT both initiates and accelerates this self-reparation, which indeed can be difficult to scientifically prove.
Deferring effect
A "troublesome" patient is often invited for the check examination only after undergoing about ten procedures, and "hopefully will be better then». This way of thinking is immoral, unethical and discreditable to a specialist, but nevertheless most of the existing prescriptions of PT unfortunately belong to this category. In some surgeries the patients are even told that the effect of the chosen PT will come only after several months (!) This means that the physician fully relies on the organisms self-reparation abilities. Indication of PT then should not be based only on the diagnosis, especially if the diagnosis is confusing, e.g. periarthritis humeroscapularis etc.
The attending physician should know the answers to the following questions: • What is the cause of the complaints, i.e. usually pain? • Is the defect functional or organic • Where was the defect initiated – where is (are) the key area(s)? • Which of the above-mentioned effects of PT is the most important for the patient at the moment? • Is there not a risk of aggravation or organification of the functional defect after the chosen PT? By these answers the physician should choose the type, location, intensity, frequency and total number of treatments. Also in relation to them, the date of the check-up examination for the patient.
7.3.3. CONTRAINDICATIONS FOR ELECTROTHERAPY[edit | edit source]
• active TB • allergy to the solutions used for moistening of the electrode sponge covers • application in the area of heart or eyes • pacemaker • cardiovascular diseases • cochlear implants • metal implants and/or malignancies in the current path • skin defects and inflammations • bleeding • menstruation • tumours • defects of sensitivity in the point of location of the electrode • psychopathological syndromes and organic psycho-syndromes • multiple sclerosis • pregnancy • inflammations of veins and lymphatic paths
7.3.4. ELECTRO-DIAGNOSTICS[edit | edit source]
Electro diagnostics Electro-diagnostic testing had its beginning in the mid to late 1800s. An excellent historical review of traditional electrical evaluation techniques may be found in Sidney Licht’s “Electro-diagnosis and Electrotherapy”. The early recognition of motor point by Duchenne in 1870, and the later mapping of these points by other scientists were major steps in the development of electrical testing.
Motoric point is a small area overlying a muscle where a slight visible contraction is most easily elicited with a minimal - amplitude (intensity) electrical stimulus. The normal motor point is usually located near the proximal portion of the muscle belly. As instrumentation and understanding of electrophysiology developed during these early years The strength - duration curve procedure and measurement of chronaxy were described and used on laboratory animals. Adrian reported using these electro diagnostic techniques on humans in 1916. Strength - duration curves, chronaxy measurements, and other electrical tests gained importance with their frequent use in evaluating peripheral nerve injuries during the two world wars. The tests are valuable when performed by skilled and experienced professionals. Their clinical use diminished, however, as newer technology provided electromyography and nerve - conduction testing. An understanding of the electrophysiological rationale of traditional tests is essential to understand contemporary electrical testing, and for intelligent and effective application of electrotherapeutic techniques.
CONTRAINDICATIONS AND PRECAUTIONS All traditional electrical evaluation tests require similar safety precautions and are contraindicated in the same circumstances. Electrical stimulation may interfere with the sensitivity of pacemakers and should not be used with patients depending on these cardiac - regulating device. Electrical stimulation should not be used over the carotid sinus, because the stimulation may induce cardiac arrhythmia. To avoid the possibility of cardiac arrhythmia or fibrillation, electrodes should not be placed so the path of electrical current passes across the heart. The effect of electrical stimulation on the developing fetus, and on the pregnant uterus has not been determined. Therefore, stimulation should not be applied over the abdominal area during pregnancy.
TRADITIONAL CLINICAL ELECTRICAL EVALUATION TESTS
1. Reaction of Degeneration Test
The reaction of degeneration (RD) test is a useful screening procedure for assessment of problems that may involve lower motor neurons. Normally innervated muscle will respond with a brisk twitch when stimulated with a short - duration pulse lasting less than 1 ms and also when stimulated with longer pulse durations, for example 100 ms. If the pulses are applied in rapid succession, the muscle will respond with a sustained or tetanic contraction. In contrast, a muscle that has lost its peripheral innervation will not respond to a stimulus of 1 ms or shorter but will contract in a sluggish manner when the longer pulse duration stimulus is applied. When performing RD, the electrode is used to search as precisely as possible for the motor point of the muscle of interest. The motor point area is first stimulated with a series of short - duration (less than 1 ms) pulses. The stimulus is applied at a frequency greater than 20 Hz which would be expected to produce a tetanic or sustained contraction. A monophasic or biphasic waveform may be used. If a monophasic or asymmetrical biphasic waveform is used, the negative (cathode) electrode is used as the active stimulating electrode over the motor point. If a tetanic response occurs, the muscle has intact peripheral innervation. If no response or a sluggish response occur, peripheral denervation is likely. The second part of the classical RD test is stimulation of involved muscle with a long - duration pulse. This may be done with a make and break key of the pencil - type electrode using a stimulator that will automatically provide a monophasic pulse of at least 100 ms duration and preferably longer. A slow or sluggish response to this part of the test indicates that contractile muscle tissue is present but that the muscle is either partially or completely denervated. The RD test is usually not done until at least 10 days after onset of the problem, so that the process of neural degeneration can progress to a stage in which electrical changes would appear. An abbreviated form of the test for reaction of degeneration may be used as a quick screening test for differentiating a muscle with normal peripheral innervation from a muscle with peripheral denervation. The RD test is only a gross screening procedure and should not be expected to differentiate or precisely identify the location of pathology. The test may be indicated in conditions of unexplained paralysis.
2. Strength - duration (i/t) curve and chronaxy test
Stimulation of denervated muscles is usually preceded by diagnostics of neuromuscular junction, and irritability of the muscle. This diagnostic test is presented in i/t (Hoolweg curve) This i/t or “strength – duration” curve and chronaxy measurements were widely used for electro-diagnosis of peripheral nervous system disorders in the past. Their frequency of use sharply declined with the development of nerve conduction testing and electromyography. When performed by the clinician experienced in strength - duration (S -D, intensity/time, i/t) curve and chronaxy measurements, these tests provide reliable means of assessing the location, severity and progress of peripheral motor - nerve degeneration and regeneration. The S - D curve has the limitation of providing data to evaluate neuromuscular integrity in the local fibers responding to the stimulus. This limitation can only be overcome by testing several muscles in the innervated by the nerve of interest. The three concepts of intensity, pulse duration and rise in time of the electrical stimulus is described in the preceding section on neurophysiologic principles of electrical evaluation. They are emphasized here, and now they take on quantitative values. Excitable tissue will respond by discharging an action potential only if an applied electrical stimulus meets certain criteria of intensity (amplitude or strength), pulse, duration and time. The intensity of the stimulus must be strong enough to depolarize the membrane to its threshold level for excitability, and in addition, the stimulus must be of sufficient duration to overcome the capacitance of the membrane.
[[|framed|center|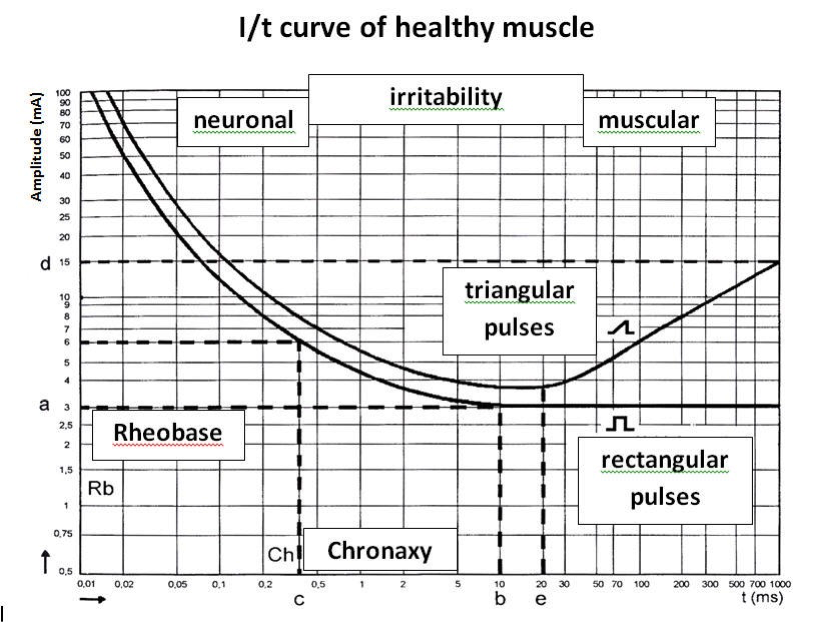 ]]
]]
Rheobase - a minimal intensity of stimulus amplitude (strength), required to elicit a minimal visually perceptible muscle contraction (for 1000 ms impulse) OR the minimal strength of an electrical stimulus of indefinite duration, that is able to cause excitation of a tissue e.g. muscle or nerve.
Chronaxy - minimal pulse duration of stimulus of twice rheobase strength that will cause the excitable cell membrane to discharge OR the shortest duration of an effective electrical stimulus to nerve or muscle tissue, having strength equal to twice the minimum strength required for excitation.
Plotting an S - D curve and determining chronaxy values require an electrical – stimulation instrument capable of producing square - wave monophasic pulse of at least 10 selectable, precise pulse durations ranging from 0.01 to 1000 ms. When collecting data for an S – D curve, the motor point or area of greatest electrical sensitivity must be precisely located with the negative (cathode) stimulating electrode. Using progressively shorter pulse durations, the value of stimulus amplitude which produce a minimal muscle contraction are recorded and then plotted onto the graph. Chronaxy and rheobase can be determined from the S - D curve. Normal chronaxy is less than 1 ms and usually are 0.1 ms or even less. Chronaxy for fully denervated muscle may be 30 to 50 ms. Strength - duration curve and chronaxy measurement have been used for evaluation of a variety of lower motor neuron pathologies. Their greatest value is for assessment of peripheral nerve injuries. Good judgement is required to plan the examination so that possible neuroanatomical sites of lesions in peripheral nerve plexus can be differentiated. When skillfully performed, these tests can provide reliable and accurate information regarding the status of peripheral innervation and denervation. S - D curve and chronaxy testing are as objective as nerve conducting testing and electromyography, are non-invasive and can provide valuable information on the status and progress peripheral nerve injuries. Other applications of the S - D curve and chronaxy are evaluation of peripheral neuritis, other peripheral nerve diseases that may involve axonal degeneration and motor neuron disease conditions. The tests may be used to complement other evaluative procedures in differentiating between normal nerve tissue and neuropathology.
3. Nerve conducting tests
The purpose of nerve conduction testing is to assess the time and quality of the conduction of neural impulses in peripheral motor and sensory nerves. A controlled monophasic pulsed electrical stimulus is applied to the skin overlying a nerve. Instruments needed for nerve conduction testing includes a differential amplifier capable of detecting accurately amplifying signals in a range from 2 microV to 50 mV. An electrical stimulator that provides square wave monophasic pulsed stimulus from 0.05 to 1 ms and output amplitude up to 500V or 100 mA, synchronized with the sweep of a storage oscilloscope. Oscilloscope is an instrument which can be used to identify and verify the characteristics of electrical signals. The stimulus frequency capability should be variable from single to pulse trains of 50 Hz. Responses from specific sites of interest, which may be from muscle in motor nerve conduction tests, from peripheral sensory nerves or from the scalp in evoked potential studies are recorded. It is distinguished in the following tests: motor nerve conduction, f - wave nerve conduction, sensory nerve conduction, h - reflex response. These tests are useful in establishing or ruling out the presence of a peripheral neuropathy and determining and localizing a peripheral nerve entrapment or a plexopathy. Another feature of the assessment of a nerve conduction test results is differentiation, which is possible when nerve conduction changes consistent with a demyelinating process and those seen with an axonal disorder.
4. Clinical electromyography (EMG)
EMG is an assessment, which provides a mean of monitoring and evaluating electrical activity of muscle directly without artificial stimulation. An advantage of EMG over the other procedures is that characteristics of muscles during relaxation and voluntary contraction can be studied. The most valuable contribution of EMG is its usefulness in evaluating electrical activity of lower motor neurons and muscle fibers. Electromyography help us identify electrical changes consistent with pathologic processes in these anatomic areas. The instrumentation required for EMG is basically similar to that used in nerve conduction testing, but an electrical stimulator is not needed. A sterile needle electrode is inserted directly into the muscle and endogenous electrophysiological activity produced by depolarization and repolarization of the muscle cell membrane is transduced from the electrode and displayed on oscilloscope. Monopolar and concentric needle electrodes are most commonly used in routine EMG. Electromyographic activity is studied under the following conditions: while the muscle is at rest, that is completely relaxed. During a mild contraction, just strong enough to produce individual motor unit action potentials, and during a very strong contraction, held with enough force to recruit as many motor units as possible.

