Coeliac disease
Coeliac disease (celiac sprue, gluten/gluten-sensitive enteropathy) is an immune-mediated, inflammatory systemic disease caused by gluten in certain cereals (and prolamins similar to it in genetically susceptible individuals). Celiac disease has a heterogeneous clinical picture and can be asymptomatic. In children, gastrointestinal symptoms, failure to thrive, growth failure and iron deficiency anaemia predominate. The diagnosis is based on the detection of antibodies to tissue transglutaminase type 2 (anti-TG2), which plays a role in the pathogenesis of celiac disease.90% of patients with celiac disease have HLA-DQ2 and the remaining 10% have HLA-DQ8 haplotype[1].The causal therapy is a lifelong gluten-free diet.
Epidemiology[edit | edit source]
The prevalence in Europe and the USA is 3-13 cases per 1000 children under 15 years of age.
The prevalence in first-degree families is 8-18%, and in identical twins it is approximately 70%.
The prevalence in the Czech Republic is approximately 1:250-300 across the age spectrum. Women are more often affected.
Etiopathogenesis[edit | edit source]
The basis of the disease is a genetic disorder of mucosal immunity. It reacts abnormally to gluten and prolamins found in wheat and other cereals.
Cereal grains contain a variety of proteins. These include, for example, albumins and globulins. Gluten is a group of proteins that includes glutenins and prolamins. The formation of antibodies responsible for celiac disease is mainly induced by the structures of gliadin, the prolamin of wheat. Similar proteins from other cereals (rye or oats) may also have similar effects.
When gluten components penetrate the intestinal mucosa, they are deaminated by tissue transglutaminase. Antibodies are then formed in the lymphoid tissue of the gastrointestinal tract (GALT) that have cross-reactivity to the enterocyte antigens of the intestinal mucosa.
The damage to the intestinal mucosa itself occurs with the participation of T-lymphocytes. The result is mucosal atrophy with impaired absorption.
The role of tissue transglutaminase[edit | edit source]
Tissue transglutaminase is an enzyme that plays a key role not only in the pathogenesis and diagnosis of disease. Gliadin and its fragments contain a high proportion of glutamine. This makes it a very good substrate for transglutaminase.
Tissue transglutaminase is found in the endomysium. It modifies a 33 amino acid long portion of gliadin with the sequence -PQPQLPY-, which it deaminates to -PEPELPY- (i.e. glutamine residues are deaminated to glutamate). This produces a structure that binds to the surface glycoproteins of HLA-DQ2/DQ8 positive immunocompetent cells. This triggers an immune response and IgA and IgG class antibodies are formed against the tissue transglutaminase. Tissue transglutaminase is therefore the intrinsic autoantigen of celiac disease.
Clinical picture[edit | edit source]
The active form of celiac sprue is characterized by clinical manifestations of varying intensity, antibody positivity and pathological findings on the small intestinal mucosa when in contact with gluten. The ratio of gastrointestinal to extraintestinal symptoms tends to be 1:1.
Gastrointestinal manifestations:
- Recurrent abdominal pain, nausea, vomiting, flatulence, failure to thrive with weight loss, constipation.
- Chronic diarrhoea and failure to thrive when dietary gluten is present (about 5% of children with celiac disease)
Extraintestinal manifestations:
- Frequent: fatigue, osteopenia/osteoporosis, smaller stature, enamel hypoplasia of definitive dentition, pubertas tarda, anemia unresponsive to therapy, dermatitis herpetiformis Duhring
- less common: hepatopathy, arthritis, epilepsy with occipital calcifications.
Other forms are not commonly diagnosed and account for almost 80% of cases, which are schematically divided into other groups:
Clinically silent form of celiac disease
It is characterized by the presence of antibodies and a typical histological picture on enterobiopsy. Although celiac disease is not clinically manifest, a lifelong gluten-free diet is fully indicated.
The latent form
We demonstrate antibodies to tissue transglutaminase, but the mucosal architecture at enterobiopsia is normal.
Potential form
This term is sometimes used to refer to a population with a genetic predisposition, i.e. HLA DQw2 antigen, and an increased number of intraepithelial lymphocytes or g/d IEL sybtypes. The prevalence is approximately 1:100 in both children and the adult population according to studies conducted in 2003.
Diagnostics[edit | edit source]
Diagnosis of celiac disease is based on history and clinical manifestations. However, especially extraintestinal forms of celiac disease may have bland and atypical manifestations; celiac disease then appears as a differential diagnosis to other diseases in the diagnostic considerations.
Screening for celiac disease is based on laboratory detection of IgA class antibodies to transglutaminase (TTG) and endomysium (EMA)
- TTG IgA has a sensitivity of 96-100% and specificity of 84-100%
- EMA IgA have a sensitivity of 88-100% and specificity of 91-100%.
A condition for screening based on the determination of these antibodies is a normal level of total IgA immunoglobulins. With a deficiency of total IgA, the determination of antibodies to tissue transglutaminase of the IgG class is carried out.
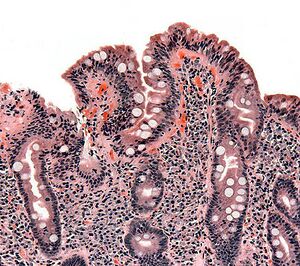
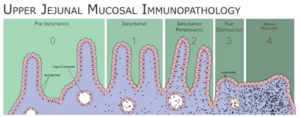
The decisive examination for the diagnosis of celiac disease is the histological finding from the biopsy of the mucosa of the small intestine. The sampling should be performed before starting a gluten-free diet. The biopsy is performed at the duodenojejunal junction or during gastroscopy. Histologically, the sample is evaluated by the Marsh method - the morphology and number of villi and crypts of the mucosa and the presence of intraepithelial lymphocytes are evaluated.
The diagnosis of celiac disease is supported by the clinical and serological response to a gluten-free diet. The diagnosis of celiac disease can be considered certain if the histological findings are positive, the patient responds to the introduction of a gluten-free diet and his age is above two years.
Only a very small number of patients develop celiac disease before the second year of age. In this case, the histological finding of intestinal mucosal atrophy alone is not sufficiently reliable (e.g. it may be an allergy to cow's milk protein) and needs to be supported by further investigations.
Diseases associated with celiac disease[edit | edit source]
Celiac disease is often associated with other autoimmune diseases, especially type 1 diabetes mellitus and autoimmune thyroiditis. Patients with morbus Down, Turner syndrome and Williams syndrome are more commonly affected. Some patients have selective IgA deficiency.
Coeliac-associated diseases in childhood:
- type 1 diabetes mellitus, juvenile idiopathic arthritis, IgA nephropathy, IgA deficiency, autoimmune thyroiditis, autoimmune hepatitis, Down syndrome, Turner syndrome, Williams syndrome.
Treatment[edit | edit source]
The basis of treatment is a lifelong strict gluten-free diet - complete exclusion of wheat, rye, barley and oats.
Sick people need to be monitored. As a rule, autoantibody levels are determined once a year. If the diet is followed, the titre decreases during the first six months.The aim of the dispensary is also to detect any associated diseases early.
Complications of untreated celiac disease[edit | edit source]
Untreated celiac disease leads to disorders caused by poor absorption of nutrients and micronutrients, but also to other disorders whose pathogenesis is not always clarified. Typical are disturbances in somatic development (growth retardation, puberty), osteopathy, anaemia and reduced school and work performance. Women suffer from fertility disorders. There is an increased risk of psychiatric illness. There is also a significant increase in the incidence of malignancies, especially lymphomas.
Summary video[edit | edit source]
https://www.wikiskripta.eu/w/Soubor:Celiac_disease.webm
Links[edit | edit source]
Related artickles[edit | edit source]
Used literature[edit | edit source]
- FRASER, JS, AL KING a HJ ELLIS, et al. An algorithm for family screening for coeliac disease. World J Gastroenterol [online]. 2006, vol. 12, no. 48, s. 7805-7809, dostupné také z <https://www.wjgnet.com/1007-9327/12/7805.pdf>. ISSN 1007-9327.
References[edit | edit source]
- Nekompletní citace článku. BODIS, Gergely, Victoria TOTH a SCHWARTING. Rheumatology and Therapy [online]. 2018, roč. 5, vol. 5, s. -, dostupné také z <https://link.springer.com/article/10.1007/s40744-018-0100-z>.
- ↑ Skočit nahoru k:a b FRÜHAUF, Pavel, Jiří BRONSKÝ a Petr DĚDEK, et al. Celiakie - doporučený postup pro diagnostiku a terapii u dětí a dospívajících. Pediatrie pro praxi. 2016, roč. 17, vol. 3, s. -,
- ↑ Skočit nahoru k:a b c d e f g h i j k l FRÜHAUF, Pavel. Celiakální sprue. Pediatrie pro praxi [online]. 2007, roč. 8, s. 333-335, dostupné také z <https://www.pediatriepropraxi.cz/>. ISSN 1803-5264.
- ↑ KOHOUT, P. Novinky v bezlepkové dietě. Interní medicína [online]. 2008, roč. -, vol. 3, s. 113-116, dostupné také z <http://www.solen.cz/pdfs/int/2008/03/03.pdf>.
- ↑ Tlaskalová-Hogenová H., Tučková L., Štěpánková R. et al. Imunopatogenetické mechanismy celiakie. Trendy soudobé pediatrie 1, Galén 1999, 181-197.
- ↑ Skočit nahoru k:a b c Se souhlasem autora převedeno z http://www1.lf1.cuni.cz/~kocna/
- ↑ ČSKB,. Cílený screening celiakální sprue [online]. ©2009. [cit. 2010-05-31]. <http://www.cskb.cz/cskb.php?pg=doporuceni>.
- ↑ WEST, J, et al. Seroprevalence, correlates, and characteristics of undetected coeliac disease in England. [online]. ©2003. [cit. 2006]. <https://www.ncbi.nlm.nih.gov/pubmed/12801951?dopt=Abstract>.
- ↑ SANDERS, DS, et al. A primary care cross-sectional study of undiagnosed adult coeliac disease. [online]. ©2003. [cit. 2006]. <https://www.ncbi.nlm.nih.gov/pubmed/12655262?dopt=Abstract>.
External links[edit | edit source]
- www.celiak.cz
- www.bezlepkovadieta.cz
- www.celia-zbl.cz
- Prof. MUDr. Nevoral J.: Cílený screening celiakie (2010)
- doc. MUDr. Kohout P., CSc.: Novinky v bezlepkové dietě (2008)
- MUDr. Prokopová L.: Celiakie - co má vědět ambulantní internista (2008)
- B-lymfom u pacientky s céliakií – obrázky