Cardiac cycle
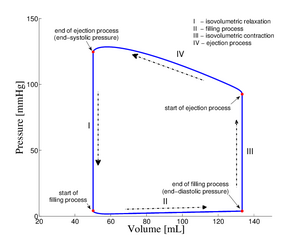
The cardiac cycle describes a single cycle in which systole (contraction of the myocardium) and diastole (relaxation of the myocardium) alternate periodically. The different phases are characterized by pressure and volume changes in the ventricles.
Phases of the cardiac cycle[edit | edit source]
Filling phase[edit | edit source]
It includes atrial systole and late ventricular diastole, where the ventricles are filled with blood. Pressure in the ventricles is (almost) constant, but the volume is increasing. The intraventricular pressure drops to zero during this phase (diastolic pressure of the ventricles), rising slightly during filling (up to 16 mmHg) - final (end) diastolic pressure in the left ventricle). The blood is driven by the inertia of the blood flow and positive pressure in the atria (maximum 16 mmHg) into the ventricles (the pressure drops almost to zero). There are three successive phases:
- phase of rapid filling of the ventricles (accumulated blood from the atria suddenly flows into the ventricles in a short time),
- the slow ventricular filling phase (blood from the veins flows through the atria and open valves straight into the ventricles),
- atrial systole.
This pumps blood from the atria into the ventricles, ends ventricular diastole and begins the next phase. Normally, atrial systole contributes little to ventricular filling (about 8%). However, it becomes more important at elevated heart rates when diastole becomes shorter and without atrial systole there would be insufficient filling of the ventricles. It lasts 400-500 ms.
Phases of isovolumic contraction[edit | edit source]
Ventricular volume does not change, intraventricular pressure increases. This is the first part of ventricular systole. Myocardial contraction occurs. The onset of contraction appears on the ECG as the peak of the R-wave. The semilunar valves close, which we hear as systolic echo. Ventricular pressure continues to rise due to myocardial contraction around incompressible fluid. Phase duration 60 ms.
Ejection phase[edit | edit source]
The pressure in the chambers does not change, the volume decreases. The final part of ventricular systole occurs when ventricular pressure exceeds the diastolic pressure in the aorta (80 mmHg) and the lungs (10 mmHg). Semilunar valves open and ventricular contents are expelled into the arteries. Maximum pressure in the left ventricle is 120-140 mmHg (up to 300 mmHg under load), in the right 20-30 mmHg. The volume of the ventricles is the expulsion of the heart rate to a minimum value. After reaching a lower value of pressure in the ventricles than in the arteries, the semilunar valves close. Phase duration 200 ms. An important term is ejection fraction: EF = SV / EDV (stroke volume/end diastolic volume). It indicates the mechanical function of the left ventricle, physiologically EF is greater than 60%.
- With the ejection of blood from the ventricles into the aorta, two phases can be described: first, the ejection is fast - the so-called fast ejection phase, then it slows down - the so-called slow ejection phase.
Isovolumic relaxation phase[edit | edit source]
It occurs after ventricular contraction has peaked. Intraventricular pressure' gradually decreases, semilunar valves close. Once they close, ventricular pressure begins to fall rapidly without changing ventricular volume. It lasts 50 ms and ends when the pressure in the ventricles drops below the pressure in the atria (the valves open and the next filling phase occurs).
Contractions[edit | edit source]
The Myocardium is similar to the skeletal muscle in its mechanics of contraction. In the heart, there is isotonic contraction (tension does not change, but the length of the muscle shortens) - a change in the volume of the ventricles at the same force of contraction, and isovolumic contraction - a change in the force of contraction of the ventricles at the same volume filling. Two types of loads are distinguished:
- afterload - the load on the myocardium during the transition from isovolumic contraction to isotonic contraction (pressure to open the semilunar valves),
- preload - the load on the relaxed myocardium that determines its initial length for the start of contraction (pressure at the end of filling).
Links[edit | edit source]
References[edit | edit source]
- ↑Jump up to:a b c d e f g h i KITTNAR, Otomar and ET AL .. Medical physiology. 1st edition. Prague: Grada, 2011. 790 pp. 211-215. ISBN 978-80-247-3068-4 .
- ↑ TROJAN, Stanislav, et al. Medical physiology. 4th edition. Prague: Grada, 2003. 772 pp. 240. ISBN 80-247-0512-5 .
Related Articles[edit | edit source]
- Heart muscle contractions
- ECG
- Systolic blood pressure
- Diastolic blood pressure
- Frank-Starling mechanism
Used literature[edit | edit source]
- TROJAN, Stanislav, et al. Lékařská fyziologie. 4. vydání. Praha : Grada, 2003. 772 s. s. 239-245. ISBN 80-247-0512-5.