Appendicitis (pediatrics)
Introduction[edit | edit source]
Acute appendicitis is the most common indication for intra-abdominal surgery in children. The exact pathophysiology of appendicitis is still unclear. However, there is general agreement that obstruction of the lumen of the appendix plays a role (coprolite - fecaloid, hyperplasia of the mucous membrane due to infection, presence of maggots). A typical medical history can be obtained in approximately 50% of patients, and about 1/3 of children with perforated appendicitis are sent home after the first examination with an incorrectly established diagnosis. It is very difficult to determine the correct diagnosis in infants, toddlers, mentally retarded and adolescents (see below). For every patient with abdominal pain, a thorough and targeted anamnesis and physical examination are most essential .
Clinical picture[edit | edit source]
Differences by age[edit | edit source]
- The course is typical for children of preschool and school age.
- Appendicitis in newborns is rare and clinical symptoms are completely atypical.
- Appendicitis in infants and toddlers is very treacherous, because the clinical picture corresponds more to dyspepsia or enterocolitis.
- Adolescent boys often dissimulate, while girls, on the other hand, tend to moan seriously.
Typical course[edit | edit source]
- the most common initial symptom is vague, dull abdominal pain , often localized first periumbilically
- later, nausea, vomiting, diarrhea and loss of appetite may be added (however, if these accompanying symptoms were present before the onset of pain, the diagnosis of acute appendicitis is less likely)
- intermittent or spasmodic nature of pain in appendicitis is not common
- as the condition progresses , increased body temperature, Tachycardia and leukocytosis in the blood count are added , the pain moves to the lower right quadrant of the abdomen and clinical signs of peritoneal irritation may be present (positive Plénies , Rovsing or Blumberg signs , obturator or psoat sign)
- children can protect the painful area (especially during a physical examination in bed)
- movement is also painful (antalgic posture or the patient's reaction after jumping on the spot)
Differences according to the localization of the appendix[edit | edit source]
Signs of peritoneal irritation may not be present if there is an obstruction between the appendix and the peritoneum:
- The appendix can be covered by the omentum, mesentery or small intestine, which is usually the case with the retrocecal position of the appendix.
- If the appendix is in the laterocecal position , palpation pain becomes more pronounced when the patient is on the left side.
- With subhepatic localization of the appendix, the patient's clinical condition may resemble cholecystitis.
- In the pelvic position, the appendix points into the small pelvis and can irritate the sigmoid (tenesma and diarrhea) or the bladder (dysuric problems and pollakisuria).
Complicated course[edit | edit source]
- Diffuse purulent peritonitis
- the appendix was perforated and purulent inflammation spread to its surroundings
- the patient tends to be febrile, has nausea and repeatedly vomits (may be significantly dehydrated)
- the abdomen breathes restrictedly, peristalsis is weakened or even disappeared
- the abdomen is markedly painful on palpation with relatively clear signs of peritoneal irritation
- Periappendicular abscess
- in this case, the inflammation spread to the vicinity of the appendix also after the perforation, but it was successfully limited by the formation of an abscess
- the patient is usually febrile, has nausea and vomiting
- physical examination of the abdomen shows signs of paralytic ileus
- the abdomen is slightly distended and diffusely painful, the maximum pain is in the right hypogastrium and signs of peritoneal irritation are indicated
- Three-phase course of appendicitis
- there was a perforation of the appendix and the development of a periappendicular abscess, followed by perforation of the abscess and the development of diffuse purulent peritonitis
- Periappendicular infiltrate
- an atypical and relatively infrequent form of acute appendicitis
- inflammation progresses from the lumen through the wall to the surroundings and fibrin sticks the surrounding structures to the appendix (intestine, omentum, ovary)
- anamnesis tends to be longer (10-14 days)
- paradoxically, the child's problems are not pronounced (vomiting is absent, subfebrile max.)
- in the laboratory, there is usually a slight elevation of inflammatory parameters
- during palpation of the abdomen, there may be palpable resistance of a stiffer nature in the right hypogastrium, which is clearly visible during palpation per rectum
- the diagnosis is confirmed by the abdominal ultrasound findings
Differential diagnosis[edit | edit source]
Appendicitis can mimic almost any pathological intra-abdominal process, and conversely, a number of conditions can mimic appendicitis. The differential diagnosis is thus quite broad.
- main diff. dg.
- reactive inflammation of the mesenteric lymph nodes - mesenteric lymphadenitis
- viral gastroenteritis
- other GIT etiology
- in girls
- ovarian torsion
- rupture of extrauterine tubal pregnancy
- premenstrual or intermenstrual pains
- cholecystitis and cholelithiasis
- pancreatitis
- urinary system
Therapy[edit | edit source]
The treatment of acute appendicitis is surgical and consists in the removal (so-called appendectomy) of the inflamed appendix. In children, the operation can be performed laparoscopically or classically via laparotomy.
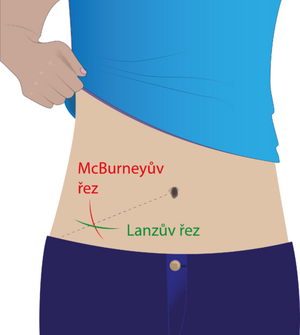
Classic appendectomy[edit | edit source]
Access to the abdominal cavity is most often chosen through an alternating incision in the right lower abdomen. This cut was first described by McBurney in 1893. This cut is often described in Anglo-Saxon specialist literature as the so-called Gridoron cut. Today, the modified McBurney cut with a more transverse course (the so-called Lanza cut) is most often chosen, while its main advantage is a better cosmetic effect. After penetrating the skin, subcutaneous tissue and Camper's layer, the fascia of the oblique abdominal muscles is crossed, the fibers of which are separated from each other by blunt dissection until the peritoneum is exposed, which is opened and the cecum with the appendix is luxated into the surgical wound (if this is possible). The individual vessels in the mesentery of the appendix are gradually ligated, which is then ligated and amputated. The stump of the cecum is traditionally plunged in and tied twice with a puncture ligature. This is followed by drying of the small pelvis and bed of the appendix,
Laparoscopic appendectomy[edit | edit source]
References[edit | edit source]
ŠNAJDAUF, Jiří and Richard ŠKÁBA. Pediatric surgery. 1st edition. Prague: Galén, 2005. ISBN 807262329X .
HOLCOMB III, George W., J. Patrick MUPRHY, and Daniel J. OSTLIE. Ashcraft's Pediatric Surgery. 6th edition. Elsevier, 2014. ISBN 145574333X .