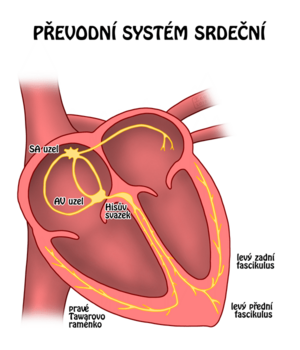
Heart rhythm disorders
Practice:
Heart rhythm disorders (arytmie, dysrytmie) is a collective name for disorders of heart rate, heart rhythm, propagation of excitement in the heart or their combination.
Classification of arrhythmias[edit | edit source]
Arrhythmias can be classified based on several aspects. According to the pathogenetic mechanisms leading to individual arrhythmias, we distinguish:
- disorders of excitability ;
- conduction disorders ;
- combined disorders;
According to the place where arrhythmias occur, we distinguish between arrhythmias:
- sinusoidal ;
- supraventricular ;
- chambered .
PAccording to the heart rate ,which the arrhythmias induce, we distinguish:
- bradycardia = bradyarytmie
- tachycardia = tachyarrhythmia
And finally, the last division reflects the clinical severity of the arrhythmias. Based on this parameter, we distinguish arrhythmias:
- benign;
- malignant.
Causes of arrhythmias[edit | edit source]
The most common cause of arrhythmia is CHD (ischemia, hypoxia, acidosis, rreperfusion injury). Then:
- ionic disorders (hypokalemia, hypomagnesia, hyperkalemia hypercalcemia);
- acid-base balance disorders;
- myocardial disorders:
- dilation or hypertrophy of the heart ( cardiomyopathy,e.g. right ventricular cardiomyopathy is directly referred to as arrhythmogenic right ventricular dysplasia);
- inflammation (myocarditis) ;
- congenital and acquired heart defects;
- disturbance of the balance of the vegetative nervous system (stress, Anxiety shock, compensation of another pathological condition);
- arrhythmogenic substances (drugs, caffeine, adrenaline alcohol, digoxin, diuretics, antiarrhythmics);
- other diseases (endocrinopathy - thyrotoxicosis);
- cardiovascular autonomic neuropathy
- next
General manifestations of arrhythmias[edit | edit source]
General manifestations of arrhythmias can be of three types:
- hemodynamic;
- electric;
- subjective.
Clinical picture[edit | edit source]
The clinical symptoms of cardiac arrhythmias include:
- palpitations;
- ↓ cardiac output per minute;
- weakness, fatigue
- vertigo
- presyncope, syncope
- stuffiness
- hypotension, shock
- angina pectoris
- Sudden cardiac death.
Diagnostics[edit | edit source]
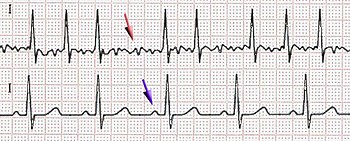
In addition toanamnesis and physical examination he diagnosis of arrhythmias clearly relies on electrocardiography (ECG),currently Telecardiology.methods can also be used . In some cases, the electrocardiographic examination is supplemented by an electrophysiological examination.
- Anamnesis.
- Physical examination.
- ECG (standard 12-lead, esophageal, stress).
- Episodic ECG recorder .
- Holter ECG (continuous ECG monitoring for 24 hours).
- Electrophysiological examination (invasive examination, introduction of sensing and stimulation electrodes into the heart cavities).
Treatment options[edit | edit source]
- Lifestyle modification.
- Pharmacological treatment (Antiarrhythmics).
- Vagal maneuvers (Valsalva maneuver, oculocardiac reflex, sinocardial reflex).
- Implantation of a pacemaker (temporary or permanent pacemaker).
- Implantation of an implantable cardioverter-defibrillator (ICD)..
- Electrical cardioversion (defibrillation).
- Radiofrequency catheter ablation .
- Surgical ablation.
Overview of Arrhythmias[edit | edit source]
By heart rate[edit | edit source]
Heart beat regularity:
Clinically by cardiac output[edit | edit source]
- With zero cardiac output - resuscitation required
- Defibrillation : ventricular fibrillationand pulseless ventricular tachycardia monomorphic and polymorphic (torsade de points),
- Non-defibrillators : Pulseless electrical activity (PEA, previously called electromechanical dissociation), asystole
- With significantly reduced cardiac output - - without treatment there is a risk of heart failure
- Extreme tachycardia - critical is the value of 220 - age of the patient, younger people tolerate tachycardia well
- Extreme bradycardia - the critical value is approximately 40, at rest a value of around 35 is still tolerated
- with normal or slightly reduced cardiac output - tolerated without treatment or with prevention of complications
- all the others
By heart rate[edit | edit source]
- Bradyarrhythmia (<60/min, cardiac output decreases at 35-40):
- sinus bradycardia, sick sinus syndrome , carotid sinus syndrome, AV conduction disorders,
- Tachyarrhythmia (>100/min, cardiac output decreases in 220-age),
- supraventricular – atrial fibrillation, atrial flutter ,atrial tachycardia, AV junctional tachycardia, AV reentry ,
- ventricular – ventricular tachycardia with pulse (and malignant arrhythmia FiK and bKT)
- extrasystoles:
- atrial,
- junctional,
- chambered.
- SVT – typically (not always) slender QRS complex, P wave morphology, can be influenced by vagal maneuvers.
- VT – typically a wide QRS complex.
According to the mechanism of formation[edit | edit source]
- Excitement disorders:
- homotopic – – sinus arrest, Sick Sinus Syndrome,
- heterotopic – extrasystoles, (triggered activity)
- conduction disorders:
- propagation of excitation by additional beam (WPW, LGL),
- conduction blocks,
- SA blockade I.–III. st.,
- AV block I.–III. st.,
- blockades of Tawar's arms ,
- Reentry (atrial, AV, ventricular),
- fibrillation (atria, ventricles), atrial flutter, tachycardia (SVT, VT).
Sinoatrial disorders[edit | edit source]
Sinus bradycardia[edit | edit source]
- Sinus rhythm with a frequency below 60/min.
- Physiologically, it tends to be lying down (especially during sleep due to increased vagal activity) or in athletes.
- Occurs during treatment with Beta-blockers, verapamil, digitalis , amiodarone. If bradycardia <50/min occurs during the active part of the day or if low MSV syndrome occurs , the dose is usually reduced.
- Other causes: sick sinus syndrom, Hypothyroidism, hypothermia , intracranial hypertension, acute myocardial infarction of the lower wall.
Sick sinus syndrome[edit | edit source]
- Symptomatic sinus bradycardia (or SA blockade) combined with SVT ,paroxysms, manifestations:
- syncope in Bradycardia,
- palpitations in SVT,
- Holter monitoringindicated ,
- treatment with permanent cardiostimulation, possibly administration of antiarrhythmics a anticoagulant treatment.
Sinoatrial block[edit | edit source]
- Loss of the P wave (and the following QRS complex), the pause corresponds to a multiple of the original PP interval,
- during longer pauses, it changes to a nodal [[A heart rhythm|rhythm](narrow QRS, inversion of the P wave, which is usually behind the QRS or is not visible at all),
- in sinus arrest, the pause does not correspond to a multiple of the PP interval.
Carotid sinus syndrome[edit | edit source]
- Symptomatic bradyarrhythmia arising as an increased response to irritation of the carotid sinus (diagnosed by massage of the sinus with a pause longer than 3 s, or. AV-blockade or hypotension),
- cardiac stimulation is indicated .
AV conduction disorders[edit | edit source]
Slowing down or stopping the conduction of impulses from the atria to the ventricles:
- proximal (AV node level ),
- distal (level of bundle of His ),
- 1st century prolongation of PQ above 0.2 s,
- II. St. intermittent AV conduction outage
- type I (Wenckebach) – gradual prolongation of PQ before failure (lack of QRS),
- type II (Mobitz) – PQ constant,
- III. St. complete block, the ventricles are activated by a junctional or nodal rhythm,
- the cause is infections (myocarditis), AMI…
- clinically manifested as ↓MSV (syncope),
- at block III. degrees and II .degrees of the Mobitz type, cardiac stimulation (temporary or permanent) is indicated .
Atrial arrhythmias[edit | edit source]
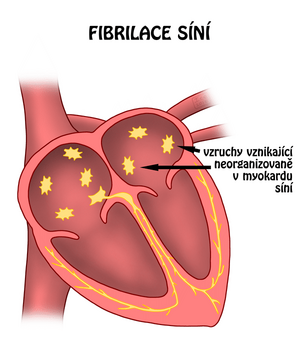
Atrial fibrillation[edit | edit source]
The most common tachyarrhythmia, caused by one or more ectopic foci and one or more reentry circuits (many functional microreentries), forms:
- first documented attack,
- paroxysmal form (ends within 48 hours),
- persistent form (ends after cardioversion),
- permanent form (chronic).
It occurs in organic heart disorders (mainly associated with atrial dilatation (mitral, tricuspid stenosis ),but also in AMI, KMP, inflammations...) and without organic disorders (hyperthyroidism…).
Clinically asymptomatic or symptomatic (palpitations, chest pain, shortness of breath, fatigue, dizziness), physically irregular, differently filled pulse, deficit between central and peripheral pulse (some contractions are not transmitted to the periphery).
On the ECG P waves are missing and instead there are fibrillation waves of different shape and amplitude, the AV conduction is irregular with a frequency of around 150/min
- Therapy
- rhythm control (restoration and maintenance of sinus rhythm),
- electrical cardioversion,
- pharmacological version of FS in sinus rhythm – antiarrhythmics IC (propafenone) and III (amiodarone, sotalol),
- maintenance of sinus rhythm – IC and III antiarrhythmics,
- rate control (optimizing heart rate to 60-80/min),
- digoxin, β-blockers, BVK (verapamil, diltiazem),
- prevention of thromboembolic complications – anticoagulant (warfarin) and antiplatelet (aspirin) treatment,
- non-pharmacological treatment,
- electroimpulse therapy (cardioversion , cardiac stimulation, implantation of an atrial cardioverter-defibrillator),
- surgical treatment ( maze procedure),
- RFA.
- treatment algorithm
- an attempt at a pharmacological version (one drug – propafenone, sotalol, amiodarone),
- in failure of cardioversion,
- prophylaxis with propafenone, sotalol (normal LV function) or amiodarone (for LV dysfunction)
- if it is not possible to carry out cardioversion or maintain sinus rhythm, drugs that slow down AV transmission (digoxin, β-blockers, BVK) should be used,
- chronic anticoagulant treatment,
- in case of ineffectiveness of RFA antiarrhythmic treatment or surgical treatment (maze).
Flutter the atrium[edit | edit source]
- the cause of macroreentry in PS defined anatomically (type I, frequency 250–350/min), less frequent is type II (functional reentry circuit, frequency 350–450/min),
- on the ECG there are QRS complexes and flutter waves - the so-called sawtooth shape - in a certain ratio (block of conduction to the ventricles in the AV node). The conversion to chambers is usually regular (e.g. 4:1), but it can also be irregular,
- cardioversion treatment, possible catheter ablation of a certain area in PS (cavotricuspid isthmus).
Atrial tachycardia[edit | edit source]
- on the ECG typically slender QRS complexes with a different configuration of P waves.
- reentry tachycardia – reentry in any area of the atria,
- automatic tachycardia – a focus of increased automation anywhere in the atrial area,
- multifocal atrial tachycardia – several foci of increased automation in the atria.
AV and junctional arrhythmias[edit | edit source]
Junctional Rhythm:
AVNRT (AV nodal reentry tachycardia)[1][edit | edit source]
AVNRT is paroxysmal supraventricular tachycardia. It typically has an abrupt start and end (jumpy rise and fall in heart rate).It manifests itself most often around the age of 30, more often in women.
The basis of AVNRT isthe reentry circuit in the area of the AV node. The arrhythmia itself is caused, for example, by supraventricular extrasystoles.
AVNRT is manifested by sudden regular and rapid heartbeat ,general weakness, chest pressure, presyncope, syncope.
Vagal maneuvers can be used to end the arrhythmiaIf they are not effective, adenosine is given . Causal treatment with catheter ablation reentry is preferred.
AV junctional tachycardia[edit | edit source]
- originates from the area of the AV junction
- non-paroxysmal junctional tachycardia – increased automaticity in the junctional region
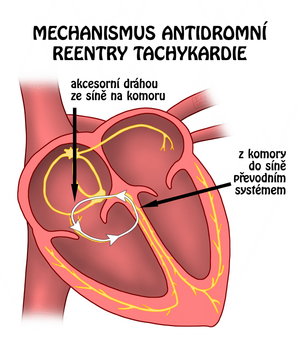
AVRT (AV nodal reentry tachycardia)[1][edit | edit source]
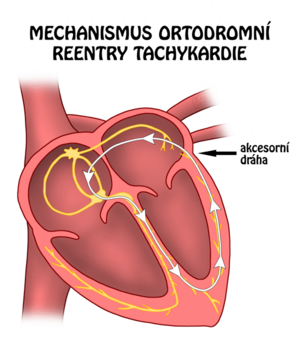
The basis of AVRT is the accessory pathway between the atria and ventricles (bundle of Kent). AVRT is part of pre-excitation syndromes (e.g. WPW with δ-wave on the ECG). Excitation conduction can be:
- orthodromic (from the atria to the ventricles, the impulse spreads through the normal path , through the normal path to the atrium by an accessory coupling );
- antidromic ( from the atria to the ventricles, the impulse spreadsthrough the accessory coupling , spreading to the atria via the AV node );
In 95% of AVRT, the excitation propagation is orthodromic.
AVRT is characterized by attacks of regular and rapid heartbeat with sudden onset and end.
On the ECG, in antidromic AVRTthe PQ interval is shortened the QRS complex is widened, and a delta wave.is present . Orthodromic AVRT appears on the ECG as regular tachycardia with slender QRS complexes.
In the case of sufficient antegrade transfer capacity of the accessory coupling and the simultaneous occurrence of atrial fibrillation ventricular fibrillation may occur.
The best prevention is RFA of the accessory pathway, class IA antiarrhythmics (procainamide, ajmaline) will also affect the transmission of the impulse in the accessory pathway.
Ventricular arrhythmias[edit | edit source]
Malignant cardiac arrhythmias without cardiac output (ventricular fibrillation and hemodynamically significant (pulseless) ventricular tachycardia with unconsciousness) require immediate resuscitation and defibrillation to restore sinus rhythm.
Ventricular tachycardia[edit | edit source]
- the presence of at least three[2] consecutive wide QRS complexes (above 0.12 s) originating in the ventricles and with a rate above 100/min
- KT can be:
- persistent (over 30 s) – non-persistent
- monomorphic (all QRS have the same shape) – polymorphic
- clinically, KT can be asymptomatic (pulsatile - especially non-persistent), but can be manifested by syncope or sudden death (pulseless - LV dysfunction), shortness of breath, angina pectoris. The term "ventricular flutter" refers to sustained ventricular tachycardia with a sinusoidal morphology with a frequency above 250/min, which is also pulseless.
- treatment of pulseless KT – defibrillation (resuscitation)
Monomorphic KT[edit | edit source]
- AMI (th. cardioversion, lidocaine)
- early KT (up to 48 hours) – as a result of functional changes of the myocardium, a frequent cause of death, but after it subsides it does not worsen the prognosis (cause – ischemia)
- late (after 48 hours) – worsens the prognosis, emergence of reentry in the marginal part of the scar, implantation of ICD
- KMP – in the prevention of sudden death, amiodarone, after sustained permanent KT ICD
- dilatational – fibrous changes in the myocardium of the ventricles will allow reentry to occur, ablation of the right bundle of Tawar is performed
- hypertrophic – high risk of sudden death
- arrhythmogenic –replacement of part of the PK myocardium with fibrolipomatous tissue, th. amiodarone, RFA
- idiopathic – does not have an organic cause, i.e. RFA
Polymorphic KT[edit | edit source]
- long QT syndrome (acquired or congenital - on on ECG torsade de pointes – rotation of the axis of the QRS complexes around the isoelectric line), th:
- acquired (to speed up heart action and shorten QT) – β-mimetic (isoproterenol) + influencing the cause(↓ K, Mg – MgSO4, effect of drugs – sotalol, macrolides, psychotropic drugs, antihistamines), possibly temporary cardiac pacing
- congenital (trigger ↑ sympathetic stimulation) – β-blockers, cardiostimulation
Ventricular fibrillation[edit | edit source]
- chaotic electrical activity leading to hemodynamically ineffective contractions of the myocardium of the ventricles, untreated leads to irreversible brain damage and death within 3-5 minutes
- on ECG the QRS complexes are replaced by irregular waves
- from non-cardiac causes, it can be caused by disturbances in the internal environment, medications, electrical interference. by current…
- treatment – Defibrillation (resuscitation)
Extrasystoles[edit | edit source]
- premature contractions arising outside the SA area
Halls[edit | edit source]
- premature P wave (usually a different morphology than a normal P wave) followed by a QRS complex of the same morphology as in sinus rhythm, no ventricular conduction may occur (premature P wave not followed by a QRS complex)
- treatment only if they are subjectively perceived unfavorably (β-blocker)
Junctional[edit | edit source]
- a premature slender QRS complex that is not preceded by a P wave (it is hidden in the QRS)
Chamberlains[edit | edit source]
- premature wide bizarre QRS complex without a preceding P wave and with a deformed T wave (it is in the opposite direction to the main QRS component), a complete compensatory pause after the extrasystole is typical (RR equality)
- R on T phenomenon – risk of developing VT or VF
Idioventricular rhythm[edit | edit source]
Idioventricular Rhythm:
- terminal stages of heart disease, when excitation occurs in the ventricles (wide, bizarre QRS complexes without P waves), during fibrinolytic therapy in AMI it is a symptom of reperfusion
Links[edit | edit source]
Related articles[edit | edit source]
- Cardiac conduction system • Vascular supply of the heart
- Heart rhythm disorders (neonatology) • Arrhythmia (pediatrics) • Antiarrhythmics
- Electrophysiological examination • Manifestations of disturbances in the generation and conduction of excitation on the electrocardiogram • Practicing the ECG
- Radiofrequency catheter ablation
- Cardiovascular autonomic neuropathy
External links[edit | edit source]
- Ventricular Tachycardia, Medscape®
- Arrhythmias (TECHmED)
- Arrhythmias (TECHmED)
- AVRT animation
- AVNRT animation
References[edit | edit source]
- ↑ a b ČEŠKA, Richard, ŠTULC, Tomáš, Vladimír TESAŘ a Milan LUKÁŠ, et al. Interna. 3. vydání. Praha : Stanislav Juhaňák - Triton, 2020. 964 s. ISBN 978-80-7553-780-5.
- ↑ COMPTON, Steven J. Ventricular Tachycardia [online]. The last revision 25.2.2013, [cit. 2013-05-28]. <https://emedicine.medscape.com/article/159075-overview>.
Sources[edit | edit source]
- PASTOR, J. Langenbeck's medical web page [online]. [cit. 2009]. <http://www.freewebs.com/langenbeck/>.
- ČEŠKA, Richard, et al. Interna. 2. edition. Praha : Triton, 2015. pp. 98-102. ISBN 978-80-7387-895-5.
| This article is a stub. You can join the authors and edit it. You can discuss the changes at discussion. |