Arrhythmogenic cardiomyopathy
Arrhythmogenic cardiomyopathy is a genetic cardiomyopathy that is characterized by fibrolipomatous myocardial replacement . The disease is manifested primarily by ventricular tachycardias , systolic dysfunction of the right / left or both ventricles, and in some cases by sudden cardiac death , which may be the first manifestation of the disease. Previously, only arrhythmogenic cardiomyopathy / right ventricular dysplasia has been defined . However, in up to 50% of cases, biventricular myocardial involvement occurs. In some cases, only the left ventricle is predominantly affected. According to the latest recommendations, the use of the more general term "arrhythmogenic cardiomyopathy" is therefore preferred.
Etiopathogenesis[edit | edit source]
The original name of the disease - arrhythmogenic right ventricular dysplasia - originated in the opinion that fibrolipomatous reconstruction of the right ventricular myocardium is a congenital heart defect. Therefore, the disease was classified as dysplasia . [1] Only further research has shown that it is a genetically determined disease .
As noted above, arrhythmogenic cardiomyopathy is a genetic disease, most commonly with an autosomal dominant type of inheritance and incomplete penentrance . Molecular-genetic basis is mutations in genes encoding proteins of intercalary disks, especially desmosomes (placophilin 2, desmoglein 2, desmoplakin and others). [1] [4] [5] As a result of desmosome involvement, other intercellular junctions are disrupted , especially gap junctions. This leads to disruption of the integrity of the affected area of the myocardium and disruption of calcium ion homeostasis. The result is mechanical and electrical instability of the myocardium, which can manifest itself in fatal arrhythmias in the early stages of the disease. Genetic mutation is detected in about 50% of cases.
Cardiomyocyte detachment is supported by increased physical exertion in affected individuals [1] . Increased physical activity leads to apoptosis and necrosis of cardiomyocytes with subsequent chronic inflammation of the affected area and its fibrolipomatous reconstruction. The rearrangement occurs because genetic mutations associated with arrhythmogenic cardiomyopathy condition suppression of Wnt signaling. As a result, fibroadipocyte progenitor cells differentiate into myocardial adipocytes .
Overall, we could divide the progression of the disease into three phases :
- Early subclinical (silent) phase, with minor structural changes in the ventricles. Already at this stage, however, desmosomes, gap junctions and the structure of sodium channels are damaged. This conditions the possibility of electrical instability of the myocardium and the development of malignant arrhythmias and sudden cardiac death. At this stage, myocardial pathologies are not apparent on imaging methods.
- In the next phase, symptomatic ventricular arrhythmias and structural and functional changes of the heart muscle develop. The right ventricle is most often affected. The area of the so-called dysplasia triangle is most often and most affected . The area delimits the right ventricular outflow tract, the area below the tricuspid valve and the right ventricular tip.
- In the next stages, fibrilipomatous myocardial remodeling progresses, leading to severe dilatation of the right / left / both ventricles (according to the location of the myocardial infarction). Small aneurysms and heart failure (right / left / bilateral) occur .
Epidemiology[edit | edit source]
The prevalence of arrhythmogenic cardiomyopathy in the population is estimated to be in the range of 1: 1000 to 1: 5000. We can observe a certain endemic incidence of the disease in the area of Venice in Italy and on the island of Naxos in Greece (hence Naxos syndrome). It is more common in men than in women in a 3: 1 ratio. The disease most often manifests itself at a younger age, when arrhythmogenic cardiomyopathy is even one of the most common causes of sudden death in young individuals and athletes (in 10 to 15%).
Clinical manifestation[edit | edit source]
In terms of manifestation, arrhythmogenic cardiomyopathy is very heterogeneous . It includes asymptomatic individuals as well as patients in whom the disease first manifested as malignant arrhythmias (ventricular tachycardias or fibrillation) or sudden cardiac death . Signs of heart failure are less common. The symptoms of patients are most often related to the development of symptomatic arrhythmias. Thus , palpitations , syncope, chest pain, etc. are observed .
Diagnostics[edit | edit source]
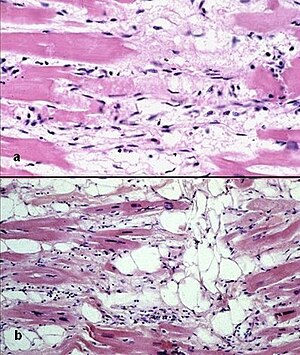
Diagnosis of arrhythmogenic cardiomyopathy is a very complex process. It is based primarily on a positive family history, deviations on the ECG and detected changes in the structure and function of the ventricles (especially with the use of echocardiography and magnetic resonance imaging of the heart). Histopathological changes of the myocardium are also examined. Part of the diagnosis is a genetic examination of mutations associated with arrhythmogenic cardiomyopathy. Already in 1994, diagnostic criteria for the diagnosis of arrhythmogenic right ventricular cardiomyopathy were introduced , which were revised in 2010 with a greater emphasis on genetic testing náhled|The picture on the right demonstrates the image of fibrolipomatous right ventricular myocardial replacement in arrhythmogenic cardiomyopathy on magnetic resonance imaging (top) and on the histopathological specimen (bottom). The ECG curves on the left show the recording of the inversion of T waves in leads V1-V4 (top) and premature ventricular contractions (bottom)
ECG[edit | edit source]
The most common ECG abnormalities are LBBB or RBBB , inverse T waves in precordial leads, QRS prolongation, and epsilon wave , which is present mainly in the more advanced stages of the disease. Various forms of ventricular arrhythmias are also observed - premature ventricular contractions and ventricular tachycardia and fibrillation.
ECHO and magnetic resonance imaging of the heart[edit | edit source]
During the examination of echocardiography and magnetic cardiac resonance, we observe changes in the structure and function of the right ventricle. This includes its dilatation , regional or global kinetics disturbances with or without a reduced chamber ejection fraction . In addition, magnetic resonance imaging of the heart is a very useful tool in the case of tissue characteristics of the myocardium, where it is possible to detect fibrolipomatous lesions in the myocardium by means of late gadolinium enhancement (LGE ). However, adipose tissue to some extent infiltrates the wall of the right ventricle even in healthy individuals.
Endomyocardial biopsy[edit | edit source]
Routine use of endomyocardial biopsy to diagnose arrhythmogenic cardiomyopathy is not recommended. [1] This is due to the fact that the test has limited sensitivity and to the fact that the interventricular septum is not usually affected by arrhythmogenic cardiomyopathy. Biopsing tissue from a free wall, especially at the right ventricle, would carry a significant risk of wall perforation and other complications.
Genetické testování[edit | edit source]
Genetic testing is recommended for diagnostic reasons and also for the needs of cascade screening of relatives . Genetic testing is relatively difficult, due in part to the considerable allelic heterogeneity of genes associated with arrhythmogenic cardiomyopathy. Nevertheless, genetic mutations associated with this disease are detected in 50-60% of cases. Soubor:ARVC E00129 (CardioNetworks ECHOpedia).webm|Parasternal projection on the long axis. Soubor:ARVC E00130 (CardioNetworks ECHOpedia).webm|Parasternal projection on short axis. Soubor:ARVC E00131 (CardioNetworks ECHOpedia).webm|Apical four-cavity projection. Soubor:ARVC E00132 (CardioNetworks ECHOpedia).webm|Apical five-cavity projection. </gallery>
Therapy[edit | edit source]
There is currently no causal treatment for arrhythmogenic cardiomyopathy. Treatment focuses on limiting physical activity , preventing malignant arrhythmias and sudden death, and treating heart failure. A higher family history of sudden cardiac death and arrhythmogenic cardiomyopathy is associated with a higher risk of malignant arrhythmias and worse prognosis. Other negative factors are the presence of multiple gene mutations, the detection of persistent ventricular tachycardia, the history of syncope, the severity of left or right ventricular dysfunction, and the occurrence of T-wave inversion in a larger number of leads.
Antiarrhythmic therapy is not always a sufficient protection against malignant arrhythmias and sudden cardiac death.Together with beta-blockers, which reduce the risk of ventricular tachycardias and slow the progression of the disease, they are rather adjunctive therapy. In patients with a history of syncope , cardiac arrest, malignant arrhythmias and decreased left ventricular function, ICD (implantable cardioverter-defibrillator) implantation is indicated , which is used in both primary and secondary prevention. In general, the indication for ICD is based on individual stratification of the risk of arrhythmic death. Catheter ablation may be used in well-tolerated monomorphic ventricular tachycardias. In extreme cases, heart transplantation is indicated.
Links[edit | edit source]
Related articles[edit | edit source]
References[edit | edit source]
- MANN, Douglas L, et al. Braunwald´s Heart Disease : A Textbook of Cardiovascular Medicine. 10th Edition edition. 2015. ISBN 978-0-323-29429-4.
- KAUTZNER, Josef. Srdeční selhání : aktuality pro klinickou praxi. 1. edition. Mladá fronta, 2015. ISBN 9788020435736.
- CORRADO, Domenico – BASSO, Cristina – JUDGE, Daniel P.. Arrhythmogenic Cardiomyopathy. Circulation Research. 2017, y. 7, vol. 121, p. 784-802, ISSN 0009-7330. DOI: 10.1161/circresaha.117.309345.
- TOMÁŠEK, Petr. , et al. Arytmogenní ventrikulární kardiomyopatie. Soudní lékařství. 2015, y. 60, vol. 4, p. 51-56,
- MCGREGOR, Stephanie M. – HUSAIN, Aliya N.. A Brief Review and Update of the Clinicopathologic Diagnosis of Arrhythmogenic Cardiomyopathy. Archives of Pathology & Laboratory Medicine. 2015, y. 9, vol. 139, p. 1181-1186, ISSN 0003-9985. DOI: 10.5858/arpa.2014-0114-rs.
- HAVRÁNEK, Štěpán. , et al. Arytmogenní kardiomyopatie levé komory. Vnitřní lékařství. 2016, y. 62, vol. 9, p. 728-735, ISSN 0042773X.
- QUARTA, Giovanni – ELLIOTT, Perry M.. Diagnostic Criteria for Arrhythmogenic Right Ventricular Cardiomyopathy. Revista Española de Cardiología (English Edition). 2012, y. 7, vol. 65, p. 599-605, ISSN 1885-5857. DOI: 10.1016/j.rec.2012.02.015.