Thromboembolic disease
Thromboembolic disease (TEN) refers to a group of thrombophilic conditions and their consequences:
- arterial thrombi and embolism,
- thrombophlebitis,
- deep vein thrombosis, postphlebitic syndrome, pulmonary embolism,
- DIC,
- mesenteric vascular occlusion.
In a narrower sense, TEN is understood primarily as deep vein thrombosis (deep veins DK) and its complications (pulmonary embolism, postphlebitic syndrome).
Pathophysiology[edit | edit source]
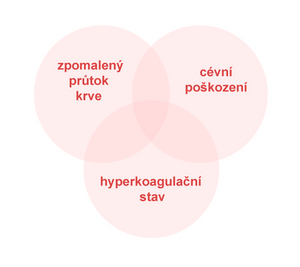
- Virchow's trias – wall damage, slowing of blood flow, hypercoagulability,
- thrombosis begins with adhesion of platelets, deposition of fibrin - white thrombus,
- a white thrombus can occlude the lumen, and stagnant blood forms a red thrombus,
- thrombosis incites inflammation in the wall leading to fibroblastic organization of the thrombus – spontaneous recanalization may occur after a few weeks, but the valves remain damaged.
Thrombophlebitis of superficial veins[edit | edit source]
Thrombophlebitis of superficial veins (thrombophlebitis superficialis) is a combination of thrombosis and inflammation of the vein wall. If the varices are also affected, it is varicophlebitis.
Causes[edit | edit source]
It is often an idiopathic disorder. It can arise iatrogenically as a result of long-term cannulation, as a result of mechanical irritation or infusion of substances that irritate the endothelium. It often arises in a pathologically changed vein (varix) or in systemic diseases (Bürger's disease, collagenoses, malignancies). Thrombophlebitis can be one of the manifestations of TEN. Less often, it is an inflammation of bacterial etiology.
Clinical implications[edit | edit source]
Redness and a painful infiltrate appear along the vein, the area around the vein is locally warmer, often also general symptoms - temperature.
Diagnostics[edit | edit source]
Thrombophlebitis can be diagnosed by clinical examination according to local inflammatory manifestations. The extent and event can be determined sonographically. simultaneous involvement of deep veins. If thrombophlebitis is near the saphenopopliteal or saphenofemoral junction, duplex ultrasonography should be performed to rule out DVT.
Therapy[edit | edit source]
It consists of:
- elimination of the cause, if known (e.g. infusion),
- cold compresses and ointments with heparin,
- general or local administration of NSAIDs,
- compression compress,
- ATBs are not routinely used in uncomplicated thrombophlebitis.
Complication[edit | edit source]
- relapses
- if the thrombus is in the junction area, complications such as DVT are common
- there is also a risk of PE in untreated thrombophlebitis of the proximal trunk of the saphenous vein
If the localization of thrombophlebitis is within 5 cm of the saphenofemoral or saphenopopliteal junction, there is a high risk of DVT or PE and anticoagulant treatment is necessary.
Deep vein thrombosis[edit | edit source]
[ ✎ edit embedded article ]
Deep vein thrombosis (phlebothrombosis) is the formation of a blood clot (thrombus) in the deep venous system leading to obstruction - restriction of blood flow through the vein.
Deep vein thrombosis primarily affects the deep venous system (veins of the lower leg, popliteal vein, femoral vein to high iliac thrombosis). It is the most common cause of pulmonary embolism. In contrast, thrombosis of superficial veins, which is usually also associated with inflammation - thrombophlebitis - does not lead to pulmonary embolism.
Pathophysiology[edit | edit source]
Video in English, definition, pathogenesis, symptoms, complications, treatment.
Under normal circumstances, there is a balance in the body between the formation and dissolution of the thrombus. A trigger factor is usually required for thrombosis to occur. The formation of a clot is thus related to the concurrence of conditions referred to as Virchow's triad :
- hemodynamic changes – mechanical compression, right-sided heart failure, aneurysm,
- violation of the integrity of the intima – mechanical vascular damage, inflammation, immunocomplexes, arteriosclerosis,
- thrombophilic conditions – imbalance of pro- and anti-coagulation factors (increased concentration of coagulation factors in plasma), mutation of genes of coagulation factors (the most common and well-known Leiden mutation of factor V).
Risk factors[edit | edit source]
There are groups of patients with an increased risk of thrombus formation, but even in such situations, some insult (immobilization, trauma, infection) is often necessary for thrombus formation.
Congenital predisposition[edit | edit source]
- Increased levels of some coagulation factors (II, VIII),
- decreased levels of protein C, protein S or antithrombin III,
- Leiden mutation,
- prothrombin mutation, dysfibrinogenemia, reduced level of plasminogen or plasminogen activators,
- hyperhomocysteinemia.
Acquired predisposition[edit | edit source]
- Dehydration - the elderly,
- reduced movement and outflow of blood from the veins – long car ride, long flight (economy class syndrome), long standing, sitting,
- smoking,
- immobilization for any reason,
- cancer (paraneoplasia - thrombophlebitis migrans in pancreatic cancer and small cell lung cancer [1]),
- surgical procedures − mainly extensive abdominal surgery, oncosurgical procedures,
- orthopedic procedures − mainly TEP joint replacements,
- hormonal changes − procoagulant effect of progesterone,
- hormonal contraception : estrogen + progesterone derivative,
- pregnancy (2nd and 3rd trimester), postpartum,
- artificial materials – valves, stents,
- injury,
- infection,
- central venous catheter (mainly risk for subclavian thrombosis),
- antiphospholipid syndrome,
- older age, obesity.
Clinical implications[edit | edit source]
Swelling of the right lower limb, livid coloration
- Swelling - caused by impaired blood drainage through the venous system from the limb,
- pain to the point of making movement impossible, with thrombosis of the deep veins of the leg there is painful dorsiflexion of the foot (Homans sign), plantar sign (painful palpation of the planta),
- increased filling in the superficial venous system, which must drain a larger amount of blood,
- livid discoloration of the limb,
- peripheral pulsations on the limb are usually preserved (deep venous thrombosis does not affect the arterial riverbed in any way, but they may be harder to feel due to swelling).
The picture of venous thrombosis on the upper limb (for example, the subclavian vein) has a similar picture - swelling, pain, increased filling of superficial veins (cephalica, basilica), most often occurs with inserted venous catheters.
Complication[edit | edit source]
Pulmonary embolism occurs when the thrombus breaks off and passes through the right heart into the pulmonary artery and its branches. This reduces the effective area of contact between capillaries and alveoli (reduced gas exchange in the lungs). If at the same time the foramen ovale in the right atrium is open, paradoxical embolization in the systemic circulation may occur.
In the venous system, after a long period of time, there is a risk of dysfunction of the venous valves and subsequent hypertension in the venous bed and venous insufficiency.
Investigation methods[edit | edit source]
- Anamnesis − we look for previous thrombosis in the patient and in his family (pulmonary embolism), in women we ask about repeated unexplained abortions (→ antiphospholipid syndrome), we also ask about the above-mentioned risk factors,
- physical examination - thorough examination of the limb (temperature - normal or warmer, circumference - increased in the affected limb, color - normal or redness, increased filling of superficial veins, peripheral pulsations - should be preserved), Homans sign (painful plantar dorsiflexion), plantar signs (painful palpation of the planta),
- imaging methods
- duplex sonography - the method of first choice, non-invasive, cheap, the venous system can be visualized along the entire length of the limb,
- venography - application of a contrast agent into the venous bed - before a suspected thrombosis, the disadvantage is the invasiveness of the examination,
- CT angiography - especially when venous thrombosis of the iliofemoral and intrathoracic veins is suspected,
- laboratory examination - D-dimers.
Therapy[edit | edit source]
The aim is to minimize the risk of embolism, prevent the spread of thrombosis and facilitate the dissolution of already formed thrombi. We place the patient in the Trendelenburg position and start anticoagulant therapy.
Anticoagulation therapy[edit | edit source]
- Low molecular weight heparins (LMWH) − are very popular especially as a prevention of thrombosis before (during and after) surgical procedures, they are also preferred in pregnant women (for warfarin contraindications). The dosage is governed by the level of risk and body weight, where appropriate, anti-Xa activity is monitored,
- unfractionated heparin - rather a drug of second choice for uncomplicated thrombosis, it is preferred when complications (embolism) are suspected. Monitoring with APTT (therapeutic value is 60-90 s),
- warfarin - the preferred drug for the long-term treatment of thrombophilic conditions in outpatients, the disadvantage is the several-day interval for inducing a therapeutic level (4-7 days). Therefore, it is recommended to combine the initiation of warfarin treatment with the administration of low molecular weight heparins. The dose of warfarin is gradually increased and, conversely, the dose of heparin is decreased, until finally it is stopped completely - based on the achieved INR, which should be 2-3,
- NOAC − currently, instead of LMWH, rivaroxaban or apixaban can be administered from day 1, which do not need to be monitored.
More detailed information can be found on the Anticoagulants page.
Thrombolysis[edit | edit source]
Thrombolysis is an excessive method that is preferred for high venous thrombosis, where there is a risk of a massive pulmonary embolism (fluttering thrombus), for younger patients without the risk of bleeding into the CNS. Tissue plasminogen activator (rt-PA, alteplase) is used.
Caval filter[edit | edit source]
In patients for whom the previous treatment is contraindicated, we introduce a caval filter. This is a small cup that is most often inserted into the inferior vena cava to trap fragments of the thrombus and thus prevent embolization. We introduce the filter endovascularly and it can be temporary or permanent. It is introduced through the jugular vein under X-ray control, below the mouth of the renal veins.
Surgical therapy[edit | edit source]
Fogarty catheter thrombectomy with expression of thrombus from the periphery of the limb is effective, but does not prevent the development of post-thrombotic syndrome. The main indication is phlegmasia coerulea dolens and impending gangrene, when it is necessary to quickly release the flow of blood. It is preferable to perform thrombectomy under general anesthesia using PEEP to avoid embolization during catheter insertion.
Interruptions of the inferior vena cava were performed in the event of a pulmonary embolism, even during anticoagulant treatment. Either the inferior vena cava was ligated under the renal veins (cavoligature) or divided into several canals with several sutures (cavoplication) or special clamps were applied. It was used earlier, today percutaneous insertion of an umbrella- or nest-type caval filter is used.
Prevention[edit | edit source]
Sufficient hydration is important non-pharmacologically, LTV is contraindicated for long-term lying down bandages.
The pharmacological path leads to anticoagulant therapy, the most used being warfarin (preventatively) and low molecular weight heparin, or unfractionated heparin (in case of threatening thrombosis).
Differential diagnosis[edit | edit source]
Phlebothrombosis is usually unilateral, bilateral is very rare.
- Swelling of the limb - involvement of superficial veins, chronic venous insufficiency, lymphedema, erysipelas, swelling after an injury,
- pain in the limb − after an injury, neurological (vertebrogenic, peripheral nerve neuropathy), acute arterial occlusion (caution − acute condition, lack of pulsation!).
- ↑ WINSTON, Tan W. Small Cell Lung Cancer [online]. ©2017. [cit. 1. 1. 2018]. <https://emedicine.medscape.com/article/280104-overview#a3>.
- ČEŠKA, Richard, ŠTULC, Tomáš, Vladimír TESAŘ a Milan LUKÁŠ, et al. Interna. 3. edition. Praha : Stanislav Juhaňák - Triton, 2020. 964 pp. pp. 230-234. ISBN 978-80-7553-780-5.
Links[edit | edit source]
Related articles[edit | edit source]
- Pulmonary embolism
- Heparin
- Leiden mutation
- Thromboembolic disease in gynecology
- Thromboembolic disease (pediatrics)
- Migratory thrombophlebitis
External links[edit | edit source]
References[edit | edit source]
- WikiLectures.eu. Deep Vein Thrombosis [online]. [cit. 2012-02-11]. <https://www.wikilectures.eu/index.php/Deep_Vein_Thrombosis>.
- ČEŠKA, Richard, et al. Interna. 1. edition. Praha : Triton, 2010. 855 pp. pp. 209-212. ISBN 978-80-7387-423-0.
- KARETOVÁ, Debora. Flebotrombóza [lecture for subject Kardiologie, specialization všeobecné lékařství, 1. LF UK]. Praha. 2010-12-17.
- BENEŠ, Jiří. Studijní materiály [online]. [cit. 29.6.2010]. <http://jirben.wz.cz>.