Evaluation of spermiogram
From WikiLectures
- Quantitative microscopic analysis of ejaculate obtained after 2-4 days of sexual abstinence by masturbation or captured during sexual intercourse in a condom made of a special material that does not damage sperm.[1]
- In recent years, there has been a permanent deterioration of the spermiogram:
- in 1951 the lower limit was 80 mil./ml, in 1964 it was revised to 40 mil./ml, in 1980 to 20 mil./ml and in 2010 WHO established 15 mil./ml as the norm.[2]
Normal spermiogram[edit | edit source]
- After 2-7 days of sexual abstinence:
- volume 1.5-4.8 ml;
- pH 7,2–7,8;
- sperm above 15 million/ml;
- total movement: 40 %
- progressive movement: 32 %
- morphology: normal forms of sperm: 4 %
Findings[edit | edit source]
If we talk about the quality/quantity of the ejaculate as such, we use the suffix - spermia, but if we want to comment on the number or characteristics of the sperm contained in the ejaculate, we use the suffix - zoospermia. It is good to be aware of this distinction in terminology, as it is often mistaken.
- aspermia – complete absence of ejaculate (no ejaculate formed or retrograde ejaculation);
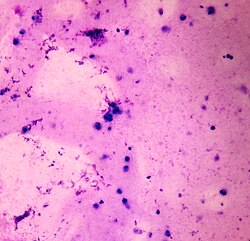
- pyospermia – leukocytes in the ejaculate;
- hemospermia – erythrocytes in the ejaculate;
- normozoospermia – parameters are within normal limits;
- oligozoospermie:
- below 15 mil./ml, the probability of fertilization may be reduced [3]
- drop below 5 million/ml – oligospermia gravis;
- asthenozoospermia – sperm movement is lower than normal, higher percentage of defective forms;
- teratozoospermia– too many morphologically abnormal sperm;
- azoospermia – sperm are absent:
- obstructive;
- testicular;
- necrozoospermia – only avital sperm are present;
- cryptozoospermia - the absence of sperm in the native sample, after centrifugation the presence of a small amount of sperm (serves to distinguish azoospermia, which most often has an obstructive etiology, from a serious disorder of the germinal epithelium)
- combination of the above pathologies: oligoasthenozoospermia, oligoasthenoteratozoospermia, asthenoteratozoospermia, oligoteratozoospermia.
Links[edit | edit source]
Related Articles[edit | edit source]
Source[edit | edit source]
- BENEŠ, Jiří. Studijní materiály [online]. [cit. 2010]. <http://jirben.wz.cz>.
References[edit | edit source]
- ↑ Gonadosan GmbH. Kvalita spermií [online]. [cit. 2011-10-03]. <https://www.fertilovit.com/cs-cz/kinderwunsch/spermienqualität.aspx>.
- ↑ http://www.sexuologickaspolecnost.cz/dokumenty/WHO_manual.pdf
- ↑ http://www.sexuologickaspolecnost.cz/vlastnosti-ejakulatu