Vestibular Schwannoma
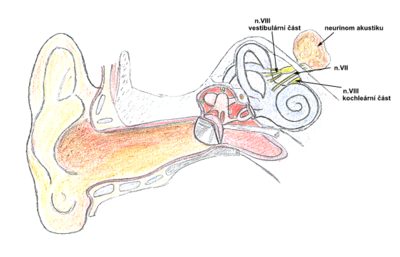
Vestibular schwannoma (acoustic neurinoma, acoustic neurilemoma, bridge cortex tumor, intracranial schwannoma) is a well-differentiated tumor originating from Schwann's sheath cells of the vestibular part of the vestibulocochlearis (statoacusticus) at the junction of the central and peripheral myelin (Obersteinich–Redlich zone). This is the most common tumor in the bridge area (meningioma or dermoid cysts may also occur in this location). Although the tumor is benign, it displaces the brainstem (especially the respiratory center in the medulla oblongata), which can acutely endanger the patient's life. Bilateral vestibular schwannoma is suspected of having AD inherited type 2 neurofibromatosis (NF2).
Classification[edit | edit source]
The Koos classification is used to determine the location and size of the vestibular schwannoma:
Koos Classification Stage I small intracanalicular tumor Stage II small tumor with protrusion into the cerebellopontine cistern (CPA); no contact with the brainstem Stage III tumor occupying the cerebellopontine cistern with no brainstem displacement Stage IV large tumor with brainstem and cranial nerve displacement
Clinical Symptoms[edit | edit source]
Clinical signs correlate with tumor size. With tumor growth, we first observe:
- hypacusis (a patient with vestibular schwannoma suffers from perceptual retrocochlear hearing loss);
- vertigo;
- tinnitus.
Also:
- Paralysis of the trigeminal nerve (n. V);
- Paralysis of the facial nerve (periferal paralysis of the VII. cranial nerve);
- intracranial hypertension syndrome;
- cerebellar syndrome.
Diagnostics[edit | edit source]
Early diagnosis is very important. See the first symptoms above. It is important to send the patient for an ENT examination. The most important examination methods include:
- tonal and speech audiometry – we show a perceptual disorder;
- BERA examination (brainstem evoked response audiometry) – we prove a retrocochlear disorder;
- MRI − the most important method for determining, possibly excluding, the diagnosis of vestibular schwannoma.
Therapy[edit | edit source]
Treatment depends on the patient's general condition, degree of hearing loss, and tumor size. In general, we distinguish 3 treatment strategies:
- Patient monitoring (Wait and scan strategy) – we monitor the patient carefully, do MRIs repeatedly, and wait for the tumor to develop. Intervention is recommended for tumor growth of 2 mm per year or more.
- Stereotactic radiosurgery using Leksell's gammaknife or LINAC accelerator. This treatment modality is indicated for smaller tumors up to 3 cm in diameter. The advantage is low invasiveness (fewer complications) and short hospital stay.
- Surgical removal is indicated for schwannomas of all sizes. The absolute indication is a large tumor that oppresses the brainstem, a tumor with a disabling vertigo or an obstructive hydrocephalus. There are 3 basic surgical approaches to vestibular schwannoma surgery:
- retrosigmoid (from the posterior fossa of the skull);
- translabyrinthic;
- infratemporal (from the middle cranial fossa).
The goal of surgery is to radically remove the tumor with as little damage to the surrounding structures as possible. Therefore, it is necessary to monitor the cranial nerves perioperatively (n. VII, n. IX, n. X, n. XI, n. XII) with the help of EMG and the cochlear part of the n. Vestibulocochlearis with the help of evoked potentials. Hearing is not possible in tumors larger than 2.5 cm in diameter. N. facialis is anatomically preserved in more than 90% of cases.
Links[edit | edit source]
External Links[edit | edit source]
Bibliography[edit | edit source]
- SAMEŠ, M. Neurochirurgie. 1. edition. 2005. 127 pp. ISBN 80-7345-072-0.
- POVÝŠIL, Ctibor. Speciální patologie. 2. edition. 2007. 430 pp. ISBN 978-807262-494-2.
- KLOZAR, Jan. Speciální otorinolaryngologie. 1. edition. 2005. 224 pp. ISBN 80-7262-346-X.
- NEVŠÍMALOVÁ, Soňa. Neurologie. 1. edition. 2002. 368 pp. ISBN 80-7262-160-2, 80-246-0502-3.