Regional anesthesia
From WikiLectures
Definition[edit | edit source]
Local application of drugs ( local anesthetics , opioids ) in order to induce anesthesia only in the desired place or body region.
Conditions and indications[edit | edit source]
Conditions :
- instruction of the patient by the anesthesiologist,
- informed consent,
- suitable anatomical conditions,
- favorable operating position,
- injection site without infection,
- physiological values of blood coagulation parameters.
Indications :
- if general anesthesia cannot be administered (poor condition of the patient, difficult intubation , patient is not hungry),
- operations on the surface of the body or during short procedures (necrectomy, AV shunt, open embolectomy, simple abdominal hernias),
- operations on the limbs (wrist and forearm fractures, as well as large joint replacements (spinal anaesthesia), in urology, in abdominal surgery),
- demanding procedures with high subsequent pain (use of a combination of general and regional anesthesia - catheter technique).
The patient comes to the operating room hungry , has intravenous access and is monitored .
Advantages :
- avoiding the risks of general anesthesia (the patient remains conscious, there is no need to secure the airway),
- price,
- the persistence of anesthesia postoperatively, or the use of a catheter for continuous postoperative dosing of anesthetic reduces the patient's consumption of intravenous and oral analgesics and enables earlier rehabilitation.
Division of local anesthesia[edit | edit source]
It is divided according to four aspects:
Place of entry of the substance into the organism :
- Topical mucosal:
- we apply to the mucous membranes with a spray (vocal tubes, trachea – lidocaine , trimecaine ),
- in the form of a gel (into the urethra – trimecaine),
- gel patches - on the skin.
- Infiltration anesthesia:
- affects the endings of sensitive fibers in the operative field,
- indications – excision, minor extirpation, simple herniotomy, tracheostomy.
- Seductive anesthesia:
- affects nerve fibers outside the area in the centripetal direction,
- it can be either regional (nerve opich), or epidural or subarachnoid ,
- often a catheter is inserted to reduce postoperative pain and enable earlier mobilization and rehabilitation of the patient.
Used product:
- natural LA very rarely – cocaine (on mucous membranes),
- synthetic local anesthetics - trimecaine, lidocaine, bupivacaine...,
- they can be combined with adrenaline (ratio 1:200,000) – reduces bleeding, prolongs the effect of the anesthetic by vasoconstricting the injection site.
Purpose:
- induction of anesthesia in the given area, enabling a painless course of the operation,
- continued analgesia in the postoperative period (catheter),
- planned combined anesthesia.
Submission technique :
- disposable needle,
- for longer-term use, a catheter is introduced - epidural, interscalene, femoral.
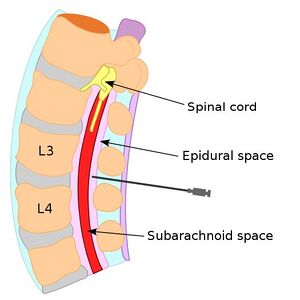
Central blockades[edit | edit source]
- subarachnoid or epidural anesthesia,
- injection site and application of local anesthetic, most often in the lumbar region,
- a combination of trimecaine + bupivacaine or opioids is used,
- indications - operations in the abdominal cavity, pelvis, bladder, prostate, DK vessels, orthopedic procedures on the hip, knees, ...,
- due to the effect on sympathetic fibers, anesthesia causes vasodilation and a rapid drop in blood pressure → it is necessary to monitor blood pressure values, administer an infusion solution (crystalloid or colloid) for volume expansion or catecholamine to increase vascular tone.
Epidural anesthesia[edit | edit source]
Technique:
- hungry sick, is pre- medicated,
- sitting position , back to the " cat's back ", or lying on the side,
- we introduce the special Tuohy cannula into the desired area of the spine slowly and carefully, we monitor the penetration into the epidural space - using the "hanging drop" or loss of resistance method,
- hanging drop method – a drop hangs from the puncture needle, after puncturing the epidural space, the drop is sucked into the cone (there is negative pressure in the epidural space) CAVE! In some cases, there may be positive pressure in the epidural space, so the loss of resistance method is preferable!
- loss of resistance method – we place a non-resistance syringe filled with physiological solution on the end of the puncture needle – when passing through the ligamentum flavum, the syringe resists, after penetrating the epidural space this resistance suddenly disappears,
- after a successful puncture, we insert the catheter about 5 cm in an overlap over the tip of the cannula,
- we administer 3 ml of anesthetic on a trial basis and wait for a reaction (exclusion of intravesal or subarachnoid catheter position),
- in the position of the catheter in the CSF or intravesally, when a larger amount of anesthetic is administered (as administered peridurally), hypotension , arrhythmia, plegia, respiratory failure would occur,
- if everything is fine, we give a full dose, up to 30 ml of local anesthetic,
- after administration of a full dose of anesthetic, we carefully monitor the patient,
- the effect occurs within 20-30 minutes,
- begins with a feeling of warmth, then paresthesia and partial motor paresis follow.
Subarachnoid anesthesia[edit | edit source]
Technique:
- the use of special needles for puncturing the subarachnoid space,
- the execution is similar to that of epidural anesthesia, but we penetrate deeper into the subarachnoid space (cerebrospinal fluid flows freely after releasing the stylet),
- the dose of anesthetic is very low 2-3 ml,
- the so-called saddle block for procedures on the perineum,
- used solutions – isobaric, hypobaric or hyperbaric,
- the distribution of anesthetic in the subdural space can be varied by positioning the patient.
Risks and complications[edit | edit source]
- bleeding,
- injection site infection,
- injuries of nerves, spinal cord up to transverse spinal cord injury ,
- hypotension , bradycardia (always have a catecholamine and a parasympatholytic drug ready),
- subsequent headache,
- with epidural anesthesia, the risk of injection into the subarachnoid space or systemic intoxication with local anesthetics.
Nerve Block and Knitting[edit | edit source]
- Use for plexus blocks or seductive anesthesia,
- large nerve bundles and stronger nerves require a higher concentration and precise targeting of the local anesthetic,
- to affect the vegetative fibers and ganglia, on the other hand, a large volume with a low concentration is needed to infiltrate as much as possible,
- the most common places of blockages:
- brachial plexus block – either axillary (axillary block), or interscalene, subclavicular (as needed for anesthesia),
- intercostal nerve block,
- sciatic nerve block - gluteal,
- femoral nerve block – in the fossa ovalis (hiatus saphenous).
Tracking and progress monitoring :
- the patient is conscious
- the anesthesiologist monitors what is happening in the operating field and monitors whether the anesthesia is sufficient, the patient's comfort, vital functions, or may induce mild sedation of the patient (midazolam, propofol).
Execution technique :
- Clarification of the main anatomical (leading) structures (muscles, bones, palpation of arteries, ...),
- careful disinfection and definition of the injection site (sterile mask),
- needle injection with stimulation by electric current or under ultrasound control,
- finding and getting close enough to the nerve (muscle response to electrical stimulation of the nerve) or under ultrasound control,
- application of local anesthetic (caution − aspirate before administration),
- catheter insertion and sterile dressing.
Risks and complications[edit | edit source]
- Failure of effect, needle breakage,
- allergic reaction - anaphylaxis, shock, bronchospasm, hypotension, ...
- immediate measures – administration of catecholamines,
- toxic reaction - euphoria, confusion, unconsciousness, convulsions, ...
- hypotension, motor paralysis, vasodilation, respiratory insufficiency,
- bleeding, nerve injury.
Links[edit | edit source]
Related Articles[edit | edit source]
External links[edit | edit source]
References[edit | edit source]
- Beneš, J., Study materials
- KRETZ, Franz-Josef – TEUFEL, Frank. Anästhesie und Intensivmedizin. 1. edition. Heidelberg : Springer, 2006. 695 pp. ISBN 3-540-62739-1.