Procalcitonin
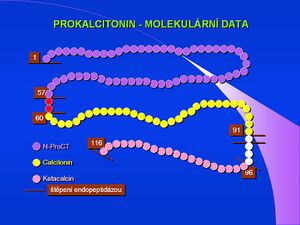
In recent years, procalcitonin (PCT) has been used as an acute phase reactant in research and clinical practice. This 116 amino acid protein, with a molecular weight of 13,000, is physiologically produced by thyroid C cells as a precursor of the hormone calcitonin. However, especially in generalized bacterial infections, other cells, mainly neuroendocrine cells of the lungs and intestines, but also cells of parenchymal organs and in sepsis practically all tissues and cell types begin to produce it. The concentration of this protein in the plasma then rises sharply. PCT released during sepsis is not converted to calcitonin. The exact physiological significance of procalcitonin is far from clear; it is thought to be involved in the regulation of inflammation and to have analgesic effects. The half-life of procalcitonin is 1 day, and after immune stimulation, its serum concentration increases about twenty-fold within 2-3 hours. The increase can be observed only in generalized bacterial, fungal and protozoal infections, it does not occur in viral infections. Less significant increases can be found in polytraumas, burns and after extensive abdominal operations.
PCT determination[edit | edit source]
It is performed by a highly sensitive immunoluminometric method, PCT-LIA (Luminescence ImmunoAssay). It is a method with two monoclonal antibodies, one against the C-terminal sequence of procalcitonin (so-called catacalcin) and the other against the central part of procalcitonin (ie against calcitonin). Anti-catacalcin antibodies are immobilized on the surface of the tube, anti-calcitonin antibodies are labelled with a luminescent probe (acridine derivative). The method requires a luminometer, it requires 20 μl of serum or plasma.
As an accelerated method, an immunochromatographic test for procalcitonin (PCT-Q) in serum and plasma is used. It requires 200 μl of serum or plasma, the result is available in 30 minutes. This test is recommended for rapid diagnosis of acute pancreatitis.
PCT guide values[edit | edit source]
Normal values (ng/ml) < 0,5; chronic inflammatory processes < 0,5–1; bacterial infection complicated by systemic reaction 2–10; SIRS 5–20; severe bacterial infections – sepsis, MODS 10–1000. Elevated PCT levels persist during prolonged sepsis, while levels of some other cytokines decrease.
Non-infectious causes of increased PCT[edit | edit source]
Postoperative condition, multiple trauma, heat injury, cardiogenic shock, in newborns the first 48 hours after birth. A comparison of PCT, CRP, IL-6 and WBC shows that procalcitonin is the indicator with the highest sensitivity and specificity for the differential diagnosis of infectious and non-infectious etiology of SIRS.
References[edit | edit source]
Related articles[edit | edit source]
- Blood
- Blood plasma
- Blood draws for testing
- Blood count
- Haemocoagulation ▪ Blood clotting test ▪ Bleeding test ▪ Erythrocyte sedimentation rate
- Biochemical blood analysis ▪ Laboratory acid-base balance test
- Hemoculture ▪ CRP ▪ PCT
Source[edit | edit source]
- With the permission of the author taken from KOCNA, Petr. GastroLab: MiniEncyclopedia of laboratory methods in gastroenterology [online]. © 2002. Last revision 2011-01-08, [cit. 2011-03-04]. < http://www1.lf1.cuni.cz/~kocna/glab/glency1.htm >.
References[edit | edit source]
- LIU, HH, JB GUO and Y. GENG. Procalcitonin: present and future. Irish Journal of Medical Science (1971 -). 2015, vol. 3, vol 184, pp. 597-605, ISSN 0021-1265. DOI: 10.1007 / s11845-015-1327-0 .
- ↑ Jump up to:a b c ÚKBLD 1. LF a VFN Praha. Procalcitonin: development of views on interpretation [online]. © 2009. [feeling. 2011-06-30]. < http://www.cskb.cz/res/file/akce/sjezdy/2009-Pha/ppt/B1/Kazda.pdf >.
- ↑ ZAZULA, R, M PRUCHA and A BURNED, et al. Procalcitonin not only in the differential diagnosis of the body's inflammatory response. Anest. intensive. Med [online] . 2002, vol. 2, pp. 86-91, also available from < https://www.prolekare.cz/anesteziologie-intenzivni-medicina-clanek?id=27121 >.
Literature[edit | edit source]
- SCHNEIDER, HG, et al. Procalcitonin for the clinical laboratory: a review. Pathology. 2007, vol 39, no. 4, pp. 383-90, ISSN 0031-3025 (Print), 1465-3931 (Electronic). PMID: 17676478 .
- RAU, BM, et al. Early assessment of pancreatic infections and overall prognosis in severe acute pancreatitis by procalcitonin (PCT): a prospective international multicenter study. Ann Surg. 2007, vol 245, no. 5, pp. 745-54, ISSN 0003-4932 (Print), 1528-1140 (Electronic). PMID: 17457167 .
- PURKAYASTHA, S, et al. Does serum procalcitonin have a role in evaluating the severity of acute pancreatitis? A question revisited. World J Surg. 2006, vol 30, no. 9, pp. 1713-21, ISSN 0364-2313 (Print), 1432-2323 (Electronic). PMID: 16927057 .
- DAMBRAUSKAS, Z, et al. Predicting development of infected necrosis in acute necrotizing pancreatitis. Medicine (Kaunas). 2006, vol 42, no. 6, pp. 441-9, ISSN 1010-660X (Print), 1648-9144 (Electronic). PMID: 16816537 .
- OLÁH, A, et al. Value of procalcitonin quick test in the differentiation between sterile and infected forms of acute pancreatitis. Hepatogastroenterology. 2005, vol 52, no. 61, pp. 243-5, ISSN 0172-6390 (Print). PMID: 15783040 .
- PAPACHRISTOU, GI, et al. Inflammatory markers of severity disease in acute pancreatitis. Clin Lab Med. 2005, vol 25, no. 1, pp. 17-37, ISSN 0272-2712 (Print), 1557-9832 (Electronic). PMID: 15749230 .
- YONETCI, N, et al. Is procalcitonin a reliable marker for the diagnosis of infected pancreatic necrosis ?. ANZ J Surg. 2004, vol 74, no. 7, pp. 591-5, ISSN 1445-1433 (Print), 1445-2197 (Electronic). PMID: 15230799 .
- RICHÉ, FC, et al. Inflammatory cytokines, C reactive protein, and procalcitonin as early predictors of necrosis infection in acute necrotizing pancreatitis. Surgery. 2003, vol 133, no. 3, pp. 257-62, ISSN 0039-6060 (Print), 1532-7361 (Electronic). PMID: 12660636 .
- PEZZILLI, R, et al. Pancreatic involvement during the early phase of shock. JOP. 2002, vol 3, no. 5, pp. 139-43, ISSN 1590-8577 (Electronic). PMID: 12221328 .
- MANDI, Y, et al. Diagnostic relevance of procalcitonin, IL-6, and sICAM-1 in the prediction of infected necrosis in acute pancreatitis. Int J Pancreatol. 2000, vol 28, no. 1, pp. 41-9, ISSN 0169-4197 (Print). PMID: 11185709 .
- Hytest. Hytest News. Procalcitonin. [online]. © 2008. [feeling. 2009-03-10]. < https://www.hytest.fi/data_sheets/newsletters/Procalcitonin%20Newsletter.pdf >.
- LÁSZLÓ, Ildikó, Domonkos TRÁSY and Zsolt MOLNÁR. Sepsis: From Pathophysiology to Individualized Patient Care. Journal of Immunology Research. 2015, vol 2015, pp. 1-13, ISSN 2314-8861. DOI: 10.1155 / 2015/510436 .
- FAN, Shu-Ling, Nancy S. MILLER and John LEE. Diagnosing sepsis - The role of laboratory medicine. Clinica Chimica Acta. 2016, vol 460, pp. 203-210, ISSN 0009-8981. DOI: 10.1016 / j.cca.2016.07.002 .