Placenta
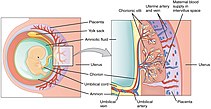
The placenta is and important organ of the femenine reproductive system. It arises by differentiation from the fetal basis of the fetal membranes, mainly from the chorion. Together with the amniotic fluid it ensures the proper development and growth of the fetus.
Anatomy of the placenta[edit | edit source]
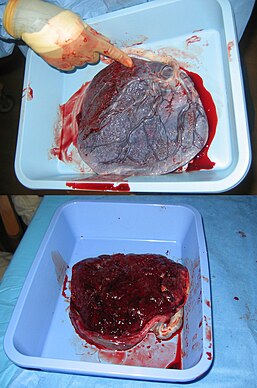
The mature placenta is a discoid-shaped vascular organ with a diameter of 15–20 cm and a thickness of 2–3 cm[1]. It weights about 500 g (17 % of the weight of the fetus)[1]; of which 50 % is maternal blood and 15 % fetal blood[1].
It is connected to the fetus by the umbilical cord (umbilicus) with a diameter of 1–2,5 cm and an average lenght of 50 cm (30–100 cm)[1]. The vessels contained within the umbilical cord (one umbilical vein, two umbilical arteries) follow a spiral course and are surrounded by Wharton´s jelly.
Development of the placenta[edit | edit source]
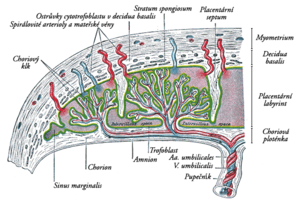
Firstly, the chorion thickens on the side facing the uterine wall and the so-called chorionic plate is developed. On the fetal side, it atrophies and forms an amniotic covering that goes into the umbilical cord.
Blood circulation of the placenta[edit | edit source]
Maternal blood is in direct contact with the villous surface of the placenta („hemochorial type of placenta“) – maternal blood bathes the chorionic vili, through which fetal blood circulates. Gases, nutrients and metabolic products are then exchanged in the chorionic villi.
Blood rich in nutrients and oxygen is supplied from the placenta to the fetus by a single umbilical vein. Albeit, the liver, to which the blood is directed, would digest all the nutrients, which is the reason why it is partially bypassed using the ductus venosus (venosus, because it connects 2 veins– umbilical vein and inferior vena cava). This allows some of the blood to enter the inferior vena cava. Pure oxygenated blood goes all the way to the liver, where it is mixed with the fetal venous blood. Therefore, oxygenated and deoxygenated blood are not differentiated in the fetus, as it is only oxygenated in the vena umbilicalis and ductus venosus. Furthermore, the blood is mixed everywhere, including in the umbilical arteries. After birth, the ductus venosus disappears and becomes the ligamentum venosum, which is an important boundary between the left and right lobes of the liver.
Function of placenta[edit | edit source]
Placental trophoblast and vascular endothelium are characterized by being semipermeable membranes which carry out active transport function. The permeablity for some substances changes during pregnancy (e.g. transfer of iron, calcium and IgG occur only during the third trimester)[1].
- Some of the most important functions of the placenta are
- Gas exchange in the blood (low arteriovenous difference – fetal oxygen transport is facilitated by fetal hemoglobin and a higher heart rate).
- Delivery of nutrients from mother to fetus.
- Excretion of metabolic waste products.
- Hormonal production: proteohormones and steroids (chorionic gonadotropin, placental lactogen, chorionic thyrotropin, estrogen, progesterone).
- Immunological barrier[1].
Placental insufficiency[edit | edit source]
- The fetus suffers from a lack of oxygen and energy sources.
- Chronic placental insufficiency – last for a significant period of the pregnancy, and it is a result of and issue in the mother or in the placenta itself.
- Causes: gestosis, hypertension of the mother, degenerative changes in the placenta[1].
- Acute placental insufficiency – is the result of complications before or during childbirth.
- May result in fetal asphyxia .
Endocrine function of placenta[edit | edit source]
The placenta is the source of hormones that maintain and support pregnancy. They include in particular:
- hCG suppresses the production of additional follicles in the ovaries and at the same time stimulates the growth of the corpus luteum, which produces estrogens and progesterone. In the fetal adrenal cortex it stimulates the production of DHEA, DHEA-S. Detection of hCG in blood or urine indicates pregnancy.
- Progesterone maintains a woman's pregnancy and stimulates breast growth. It is the initial substrate of cortisol , which is produced in the fetal adrenal glands. In male fetuses, it then develops further into testosterone in the testicles. Progesterone production first takes place in the corpus luteum, and then in the placenta. This change is carried out by a process called luteo-placental shift and it is completed by the 8th week of pregnancy.
- Estrogen is formed from the production of dehydroepiandrosterone (DHEA) in the fetal adrenal glands. DHEA is produced in this glands from progesterone, which is transported through blood from the placenta. In the next step, DHEA returns to the placenta, where it is converted into estrogen. The effects are mainly on breast growth, both directly and indirectly by increasing prolactin levels . Furthermore, they stimulate blood flow through the placenta and the production of prostaglandins. They affect the number of receptors for oxytocin in the cells of the uterine muscle. Towards the end of pregnancy, the level rises sharply and has an antagonistic effect on progesterone.
- Chorionic somatomamotropin (hCS) is also referred to as placental lactogen (HPL) and affects nutrient metabolism. It stimulates protein anabolism and lipid catabolism (lipolysis). In women, it stimulates the growth and development of the mammary gland. It increases the availability of glucose in the fetus .
- Corticoliberin´s (CRH) main function is to regulate the length of pregnancy and subsequent birth . In preterm births, the CRH level rises faster than in full term births. In the fetus, corticoliberin acts on the secretion of ACTH in the pituitary gland and also affects the production of DHEA, DHEA-S in the adrenal glands.
Links[edit | edit source]
Related articles[edit | edit source]
External links[edit | edit source]
- JĚŽOVÁ, Marta – HOTÁRKOVÁ, Sylva – MŮČKOVÁ, Katarína. Hypertextový atlas fetální patologie : Multimediální podpora výuky klinických a zdravotnických oborů [online]. Portál Lékařské fakulty Masarykovy univerzity [online], ©2008. [cit. 26.11.2011]. <http://portal.med.muni.cz/clanek-463-hypertextovy-atlas-fetalni-patologie.html>.
- SILBERNAGL, Stefan a Agamemnon DESPOPOULOS. Atlas fyziologie člověka. 3. vydání. Praha : Grada, 2004. 435 s. ISBN 80-247-0630-X.
- KITTNAR, Otomar, et al. Lékařská fyziologie. 1. vydání. Praha : Grada, 2011. 790 s. ISBN 978-80-247-3068-4.