Operative procedures on the gallbladder and bile ducts
From WikiLectures
Gallbladder puncture[edit | edit source]
- It is indicated less and less often.
- It is performed diagnostically or therapeutically.
- Intraoperatively or laparoscopically.
- Diagnostics - collection of material for culture, application of contrast for cholecystocholangiography.
Cholecystotomy[edit | edit source]
- Today it is practically carried out.
- From the removal of stones from the gallbladder in cholelithiasis.
Cholecystostomy[edit | edit source]
- When it is necessary to drain the gallbladder externally (acute pancreatitis, severe inflammation).
- If it is necessary to perform the procedure as quickly as possible for the general condition of the patient.
- After removing the stones and verifying the patency of the cystic duct - we place a stronger drain, fixed waterproof with a tobacco suture into the cholecystostomy.
Cholecystectomy[edit | edit source]
- First performed in 1882 in Berlin, here for the first time by prof. Maydl (1891).
- Oblique or transrectal incision in the right subcostal region, or from upper median laparotomy.
- We choose the antegrade or retrograde procedure:
- Retrograde procedure:
- After cutting the peritoneum at the neck, we dissect the cystic artery, ligate it, cross it,
- the same done with the cystic duct,
- we release the gallbladder from the bed towards the fundus (i.e. retrograde - we go from back to front).
- Antegrade procedure - we release the gallbladder in the opposite direction - from the fundus to the neck, until finally we ligate the ductus and artery.
- The peritoneum is sutured above the bed, a drain is placed next to the bed (drainage of bile from aberrant bile ducts, effusion, blood).
- We leave a cannula in the cyst to diagnose the patency of the tract and papilla.
Urgent cholecystectomy[edit | edit source]
- With signs of progression of inflammation, peritonitis.
- It is a life-saving performance.
Acute cholecystectomy[edit | edit source]
- Within 72 h after the onset of the disease.
- We prevent her from possible complications resulting from emergency surgery.
- Mortality is low, less than 1%.
- The danger is with an acute exacerbation of chronic inflammation - the surrounding area is all overgrown and there is a danger of injury to important structures in the area of the ligaments. hepatoduodenal (v. portae, a. hepatica, choledochus).
- In addition, these are usually old people who are not ready for surgery.
- It must therefore be well considered - there must be good equipment and staff - an X-ray is necessary, or intraoperative sonographer.
Deferred cholecystectomy[edit | edit source]
- Between the ninth and twelfth day after the onset of the disease during one hospitalization.
- Between the 3rd and the 9th day, it is not worth operating, because the area around the gallbladder is affected by inflammation, stuck together with the surrounding organs, and it would be difficult for the operator to orient himself; during this period it is operated only urgently.
- It prevents repeated exacerbations and repeated hospitalizations.
Planned (late) cholecystectomy[edit | edit source]
- At the earliest in 3 weeks during the next hospitalization.
- In the stage - "at rest" on a "chilled" gallbladder.
Choledochotomy[edit | edit source]
- Longitudinal incision of the choledochus.
- It can be performed anywhere, most often supraduodenal (the choledochus has four sections - an intamural part, a pancreatic part, a part behind the duodenum and a part above the duodenum).
- We can examine the bile ducts with a probe, forceps, spoon, endoscope
- We make the closure with an absorbable material - either primarily (simply sew it up) or, more often, we slide a T-drain (Kehr's drainage) in there.
- Drainage allows the outflow of bile after surgery, when the papilla spasms, in a few days the drain is simply pulled out.
- Although some bile will leak out through that hole, the adhesions that have formed around the T-drain will not allow it to get anywhere else... it will spontaneously close within 24 hours.
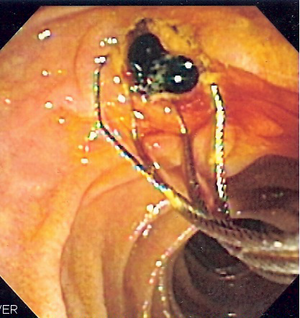
Papillotomy and papillosphincterotomy (PT + PST)[edit | edit source]
- It is performed transduodenal, after releasing the duodenum as ERCP (endoscopic retrograde cholangiopancreatography), on an introduced choledochotomy probe.
- If we cut about 0.5 cm - papillotomy.
- If we cut more, we also cut the muscle - papillosphincterotomy.
- The entire sphincter should never be crossed - reflux and cholangitis can then occur, which are difficult to treat.
Divulsion (dilation) of the papilla[edit | edit source]
- Post-inflammatory or post-traumatic narrowing of the papilla.
- Can be expanded with probes of gradually increasing diameter.
Anastomoses[edit | edit source]
- Anastomoses of the gallbladder and bile ducts:
- In case of malignant obstruction of the lower part of the bile ducts, a temporary solution for jaundice before a radical procedure.
- Connect the gallbladder or bile duct to the GIT (pars horizontalis duodeni, stomach antrum, intestinal loop).
- If the indication is a benign disease, we choose connection to a Roux anastomosis to prevent cholangitis.
- Hilar anastomoses:
- Between the rest of the ductus hepaticus communis and the excluded loop according to Roux.
- If necessary, resect the bile duct.
- Technically demanding performance, frequent complications and necessary reoperations.
- Intrahepatic anastomoses –as an emergency escape, with a tumor of the liver hilum.
- We sew the intestinal loop on the right or the stomach on the left to the wedge-shaped part of the edge of the liver.
- The excess pressure in the liver often dilates the outflow bile ducts and drains them into the GIT.
- Bile duct plastic surgery - when there is a narrowing, most often after iatrogenic lesions.
- Instead of the stenosis, we cut it longitudinally and suture it transversely, we have to create an endoplasty under it, which we place transpapillary and then remove after about half a year.
Links[edit | edit source]
- Bile ducts
- Cholelithiasis
- Cholangitis
- Jaundice
- Inflammatory diseases of the gallbladder and bile ducts
Source[edit | edit source]
- BENEŠ, Jiří. Studying materials [online]. [cit. 5.5.2010]. <http://jirben.wz.cz>.