Manifestations of inflammatory rheumatic diseases on the musculoskeletal system and their surgical treatment
Rheumatic diseases are among the most widespread human diseases. They occur in up to 30% of the population, for 3% they mean permanent disability.
Rheumatoid arthritis
Rheumatoid arthritis (polyarthritis progressiva primaria chronica) is a chronic inflammation characterized by synovial hypertrophy with infiltration by inflammatory cells, destruction of articular cartilage and bones decalcification (osteoporosis). Rheumatoid arthritis is characterized by the production of antibodies (RF – rheumatoid factor, ANF – antinuclear factors) and acute-phase proteins. Clinically, rheumatoid arthritis can be described as symmetrical polyarthritis, which predilectionally affects the small joints of the hand and radiocarpal joints with prolonged morning stiffness.
Occurence
Rheumatoid arthritis is 2-3 times more common in women. Symptoms develop mostly between the ages of 20 and 40. However, there is also juvenile rheumatoid arthritis, which primarily affects large joints.
Etiology
Rheumatoid arthritis is an autoimmune inflammation that is often associated with the HLA-DR4 or DR1 immunophenotype. The initiator is believed to be an as yet unknown microbial pathogen (EBV, retroviruses, parvoviruses, Borrelia,... are being considered). It is not known exactly which antigen the autoimmune reaction is directed against - probably against type II collagen or against cartilage glycoprotein 39 (it binds to DR4). Rheumatoid factor occurs in 80% of patients = antibodies against the Fc fragment of IgG.
Pathological-anatomical changes
The first changes are in the synovium, then in the fluid, in the cartilage and finally in the paraarticular space. At first, a serofibrinous intraarticular inflammation develops, then the pannus forms. Pannus is a villous overgrown synovial membrane, in which ligaments and blood vessels proliferate excessively. It covers the articular cartilage, separating it from the nourishing synovial fluid. As a result, chondrocytes disappear and subchondral bone mass is gradually eroded. If the pannus growing from opposite sides of the joint joins, it can further develop fibrotic changes, ossify, and finally ankylosis occurs .
Another morphological manifestation of rheumatoid arthritis are rheumatic nodules, which arise mainly in the subcutaneous tissue. Histologically, they consist of three layers:
- Necrotic tissue in the center
- A layer of palisade fibroblasts and multinucleated cells around the necrosis
- A layer of chronic inflammation in the periphery
Clinical picture
Joint damage
Symmetric polyarthritis
Initially, the joints of the hand are affected (starting from the periphery → proximal interphalangeal → “bottle fingers”; metacarpophalangeal; radiocarpal). It usually does not affect the distal interphalangeal. Later, ulnar deviation of the fingers, swan neck deformities (hyperextension in the proximal interphalangeal joint and flexion in the distal interphalangeal joint) and buttonhole deformities (flexion in the proximal interphalangeal joint and hyperextension in the distal interphalangeal joint) are typical. The joints are painful at rest, during palpation and movement. Morning stiffness (it takes more than an hour to move properly) is also typical. The joints have the classic signs of inflammation in addition to redness (rubor). In more severe cases, chronic inflammation can lead to volar subluxation of the wrist and rupture of finger tendons. The activity of the process is fluctuating, often depending on the weather.
Damage to the individual joints
- Elbow disorders - flexion contractures
- Shoulder joints – rotator cuff ruptures
- Hip joints - affected less often
- Knee joints – angular deformities and flexion contractures. Fluid may enter the popliteal bursa – Baker's cyst. On the leg, hammertoes and hallux valgus are typical findings
Spine
Affected mainly in the neck region, the involvement of the atlantoaxial joint with subluxation is severe (neck and head pain, spinal cord compression). Sudden death can also be a complication of subluxation. ![]() Before any surgery with intubation, an X-ray should be taken if atlantoaxial subluxation is suspected.
Before any surgery with intubation, an X-ray should be taken if atlantoaxial subluxation is suspected.
Impairment of the temporomandibular joint
It causes pain when chewing.
Progression of the disease
There are 3 types of the progression of the disease:
- monocyclic – one cycle of the disease followed by remission lasting more than 1 year;
- polycyclic – slowly progressing progression with episodes of incomplete remissions (most common);
- progressive – permanent progression without remissions.
Extra-articular disability
The disease can be accompanied by extra-articular disabilities:
- rheumatic nodes (under the skin, especially above the elbows and above the proximal edge of the ulna), usually multiple, usually painful nodules, up to several cm in size;
- tendosynovitis (mainly in the hands, tendon ruptures with the development of deformities – swan's neck, buttonhole);
- osteoporosis (initially periarticular, later diffuse – pathological fractures);
- secondary amyloidosis (AA, especially kidney damage);
- hematological abnormalities (mainly anemia, thrombocytosis);
- eye disorders (iritis, iridocyclitis, keratoconjunctivitis);
- damage to the skin, heart, blood vessels, nerves, lungs, etc.
Diagnostics
Laboratory finding
- Inflammatory markers (↑ FW, CRP)
- Antibodies:
- rheumatoid factor (RF) – antibody (mostly IgM) against Fc fragments of IgG, demonstrated by latex-fixation test
- anti-CCP – antibody against cyclic citrullinated peptide, are more specific for RA than rheumatoid factors
- APF – antiperinuclear factors
- ANF - antinuclear factors
- Punctate (biochemically RF, high content of polymorphonuclear cells)
X-ray findings
- Early - swelling of the soft tissues near the joints, periarticular osteoporosis, marginal erosion of the bone
- Late - narrowing of the joint space, diffuse osteoporosis, deformities, bone ankylosis
Four stages according to Steinbrocker were introduced for the evaluation of X-ray images:
| Stage | Characteristics |
|---|---|
| Stage I | periarticular osteoporosis, no destruction |
| Stage II | slight signs of destruction, no deformities |
| Stage III | destruction of cartilage and bone, deformities |
| Stage IV | fibrous or bony ankylosis |
- Furthermore, scintigraphy can be used in the diagnosis (it will show the distribution of the disability in individual joints).
Criteria for diagnosis
For the diagnosis of rheumatoid arthritis, the presence of 4 of the 7 criteria is important:
- morning stiffness
- arthritis of 3 or more areas
- arthritis in the joints of the hand (RC, MCP, PIP)
- symmetrical arthritis
- rheumatoid nodules
- rheumatoid factor (RF)
- X-ray changes
Treatment
Regime measures
In the acute stage, bed rest, prevention of contractures, antalgic splints, etc.
Physical therapy and rehabilitation
Maintaining range of motion in the joint, preventing muscle weakness.
Pharmacotherapy
The basis of pharmacological treatment are disease modifying antirheumatic drugs (DMARDs).
Disease-modifying drugs (DMARDs)
This includes two groups of drugs:
- conventional
- biological treatment
- Conventional drugs
- methotrexate – the most frequently used drug, the drug of first choice
- leflunomide – inhibitor of the pyrimidine nucleotides, has similar effects as methotrexate
- sulfasalazine
- hydroxychloroquine and chloroquine - have the weakest effect
- Biological treatment
- TNFα inhibitors – etanercept, infliximab, adalimumab, golimumab, certolizumab pegol
- rituximab – a chimeric monoclonal antibody against the CD20 molecule
- abatacept – blocks T-lymphocyte activation by blocking the costimulatory signal
- tocilizumab – an antibody against the IL-6 receptor
- anakinra – IL-1 receptor antagonist
Other medications
- non-steroidal antirheumatic drugs and analgesics - only symptomatic drugs - COX1 inhibitors - diclofenac, indomethacin, selective COX2 inhibitors - nimesulide, coxibs
- corticoids - generaly (prednisone) or intra-articular (triamcinolone) - to bridge the period until the onset of effect of DMARDs.
Surgical treatment
- synovectomy (radiation yttrium isotope application to the joint is also possible)
- total endoprosthesis
- arthrodesis (fixation of the joint in a favorable position, pain relief, most often the radiocarpal area).
Summary video
https://upload.wikimedia.org/wikipedia/commons/9/9d/Rheumatoid_arthritis.webm
Bekhterev's disease
Ankylosing spondylitis (also Bekhterev's disease or ankylosing spondylitis) belongs to spondyloarthritis, a group of inflammatory rheumatic diseases affecting the joints of the spine (intervertebral, costovertebral, SI joints, discs and ligaments of the spine, sometimes also root or peripheral joints). It leads to gradual ossification of joint capsules and ligaments and thus to ankylosis of segments and even the entire spine (it can become stiff in any position).
Etiopathogenesis
The disease begins at a young age (most often in the 2nd-3rd decade). It occurs more often in men. The disease is linked to HLA-B27. An etiologic agent has not been established. The role of intestinal microflora is considered.
Symptoms
Symptoms of the disease are divided into three groups: axial, peripheral and extra-articular symptoms.
Axial symptoms
The basic symptoms of the disease include inflammatory pain in the lower back - it arises due to sacroiliitis, typically in the second half of the night and wakes the patient. It is accompanied by morning stiffness. Both pain and stiffness improve with exercise. The pain continues to spread to higher areas of the spine (up to the cervical spine) - the basis is spondylitis. Axial symptoms also include arthritis of the shoulder and hip joints.
Peripheral symptoms
Most often, asymmetric oligoarthritis occurs with a preference on the lower limbs. Dactylitis (the so-called sausage finger ) can also occur - an involvement of the interphalangeal joints of one finger and the tendon.
Extra-articular symptoms
- eyes – acute anterior uveitis
- heart – aortic insufficiency, conduction disorders, aortitis
- GIT – ulcerative colitis, Crohn's disease
- lings – fibrosis
- kidneys – amyloidosis,
- osteoporosis of the vertebrae
Diagnostics
Physical exam
During the examination, we focus on the sacroiliac joints, the development of the spine in three planes and the expansion of the chest.
- Mennel's maneuver - we push the patient on the wings of the hip bones. The test is positive if the patient feels pain on the affected side.
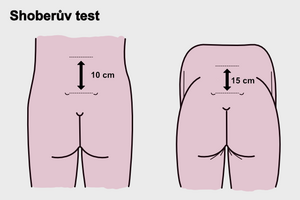
- Schober's test - Shows the development of the lumbar spine.
- Forestier's flèche – This is the distance from the occiput to the vertical wall. It should be a maximum of 2 cm.
- lateroflexion
- chest expansion – at least 5 cm
Imaging
Sacroiliitis is the first manifestation on the X-ray. Furthermore, syndesmophytes and ossification of tendon attachments are formed, which leads to the fusion of the vertebral bodies up to the image of the so-called bamboo rod. Sacroiliitis often bilateral.
We distinguish 5 stages according to the localization of changes.
| Stage | Inflammatory changes |
|---|---|
| Stage I | unilateral sacroilitis |
| Stage II | bilateral sacroilitis |
| Stage III | lumbar spine impairment |
| Stage IV | thoracic spine impairment |
| Stage V | cervical spine impairment |
Another important imaging method is MRI, where a typical finding is the presence of an effusion or swelling of the bone marrow.
Laboratory finding
In the laboratory findings, we find an increase in sedimentation and CRP. Normocytic normochromic anemia is also present.
Treatment
The basis of treatment is regular, lifelong exercise, rehabilitation and physical therapy. Spa treatment is indicated for patients every year. Pharmacological treatment includes:
- nonsteroidal antirheumatic drugs
- DMARDs – only sulfasalazine is effective in forms with peripheral arthritis
- biological treatment – TNF blocking drugs: etanercept, infliximab, adalimumab, golimumab
Rheumatoid Diseases in Children
Rheumatology surgery
- The operation often ends in failure, the cooperation of an orthopedist, a rheumatologist and a rehabilitation worker is necessary
- The primary task is the prevention of deformities - synovectomy
- Other tasks:
- To correct created deformities (arthroplasties, arthrodesis, alloplasty)
- Restore lost joint functions, relieve pain
- Wound healing is often poor (due to vasculitis)
- Poor access to intubation in spinal disorders is often negative for surgery
- Worse course of infections
- A long-term operational plan is being developed - operating on individual joints (in stages).
Links
- BENEŠ, Jiří. Studijní materiály [online]. [cit. 2011]. <http://jirben2.chytrak.cz/>.