Kidney function
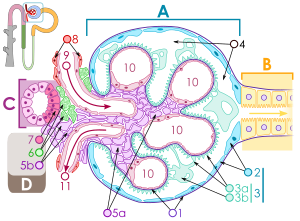
The kidneys are a paired organ housed in the retroperitoneum with several vital functions.
Exclusion functino[edit | edit source]
The kidneys excrete those substances that are in excess in the body. E.g. water sodium, potassium, phosphate and calcium ions, but also by-products of metabolism, such as uric acid, which is a product of purine metabolism, urea (as the end product of protein metabolism) and creatinine as the end product of creatine metabolism of muscles.
Endocine functino[edit | edit source]
Renin is secreted by the juxtaglomerular cells, which have been transformed from the muscle cells of the vessels lining the distal tubule. It is secreted as a response to reduced blood flow to the kidneys, to stimulation by the vegetative system or to a reduced concentration of sodium and chlorine in the distal tubule. Renin is part of the renin-angiotensin-aldosterone system, which maintains the composition of blood plasma and is involved in the regulation of blood pressure.
Erythropoietin is a substance that regulates the production of red blood cells and is largely produced in the kidneys (90-95%).
Vitamin D is converted in the kidneys to the active metabolite calcitriol. Its function is to support the absorption of calcium and phosphates in the intestine and participate in the management of calcium metabolism in bones.
Control of blood volume and blood pressure[edit | edit source]
Pressure diuresis: As soon as the volume of blood in the circulation increases, vasoconstrictino occurs reflexly in the arteries and thus the arterial pressure and filtration pressure in the kidneys increase. More glomerular filtrate is formed, secretion of hormones involved in water absorption is reduced, and urine output is increased, thereby reducing circulating volume and lowering blood pressure. Humoral regulation of blood volume: increasing blood volume in the right atrium induces the secretion of atrial natriuretic factor (ANF), which increases the excretion of sodium and, with it, water in the renal distal tubule. With increased pressure, the secretion of antidiuretic hormone and renin also decreases.
Maintenance of acid-base balance[edit | edit source]
A large amount of bicarbonate anions are filtered into the glomerular filtrate and are then actively reabsorbed as needed. Hydrogen cations are actively secreted into the tubules. The change in the size of the output of these two ions is proportional to very small changes in the extracellular concentration of these ions. As the amount of excreted hydrogen cation increases (exceeds excretion of bicarbonate), the acidity of the extracellular fluid decreases and acidosis occurs. In alkalosis, the opposite is true. Complicated mechanisms of hydrogen cation regulation cause a slow onset of effect, which occurs only after a few days. However, this disadvantage is compensated by the possibility of regulation for a relatively long time.
Links[edit | edit source]
Related articles[edit | edit source]
- Kidneys
- Calcium phosphate metabolism
- Erythropoietin
- The renin-angiotensin-aldosterone system
- Kidney function in maintaining acid-base balance
- Natriuretic peptides
Resources[edit | edit source]
- ROKYTA, Richard. Physiology for bachelor's studies in medicine, nursing, science, pedagogy and physical education. 2nd edition edition. ISV, 2008. ISBN 80-86642-47-X.

