Insulin therapy
Therapies vary widely from type to type of diabetes. While in type 1 diabetes we rely on insulin therapy, in type 2 diabetes diet or oral antidiabetic drugs are used depending on the degree of insulin resistance and insulin therapy we use in the more severe cases. The cornerstone of the treatment of type 1 diabetes is insulin substitution, which must be supplemented with alimentary and regimen restrictions.
Cooperation between the doctor and the patient is necessary since an individual treatment plan is drawn up for the patient, consisting of:
- dietary regimen with detailed instructions;
- lifestyle changes;
- education;
- psychosocial care;
- pharmacological treatment of diabetes and associated diseases;
- regular checks.[1]
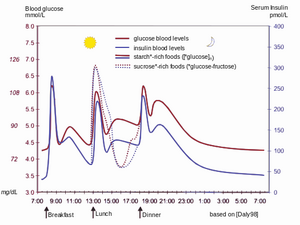
We start insulin therapy on an ambulance check or during hospitalization. We always apply a lower dose at the beginning to hypoglycaemia, as endogenous insulin secretion still persists. We collect a large glycemic profile which consists of glycemia always before and after meals, at 10 pm and at 3 a.m. at night. Based on regular glycemic profiles, we adjust the dosage to adjust the optimal compensation.
Insulins are not binding to plasma proteins in the bloodstream, so they quickly leave circulation and bind to insulin receptors. Exogenous insulin is more than 60% degraded in the kidneys, the rest of the degradation is carried out in the liver (unlike endogenous insulin, which is degraded for the most part in the liver). Only a small part of the insulin administered is excreted in the urine in an unchanged form.
Types of insulins by origin[edit | edit source]
Animal insulins are used the longest, previously isolated from beef or pork pancreas, today monocomponent and highly purified. Beef insulin differs by three, pork one amino acid from human insulin. Due to the risk of BSE beef insulins are no longer used.
Human insulin has been prepared through recombinant DNA transfer technologies to Escherichia coli. Compared to animal insulins, human insulin is a more polar substance, has faster absorption from the place of application and has shorter action. While applying human insulin will better replicate the physiological function of this hormone, we will mask some of the warning signs of hypoglycaemia that are otherwise present when we applicate animal insulins.
Insulin analogues are also used, which are biosynthetic differing in order of amino acids and pharmacokinetics.
Types of insulin according to the duration of action[edit | edit source]
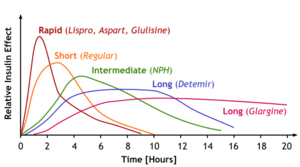
Insulins with different duration of action have been developed to compensate for diabetes properly.
Short-acting insulins[edit | edit source]
Short-term insulins are produced to cope with acute hyperglycaemia situations as well as for intensified insulin therapy as clear water-soluble solutions of crystalline insulin complexes with zinc with neutral pH. For acute intervention in case of hyperglycemic ketoacidosis coma and during anaesthesia or other extreme loads in diabetics can also be applicated intravenously, which has almost immediate effect. As part of the intensified insulin therapy, it is then applicated subcutaneously, when it works within 15-30 minutes, the peak of the action takes 1-3 hours and lasts 4-6 hours. Short-acting insulins include:
- Insulin lispro – its advantage is less propensity to produce hexamer and dimers, which facilitates absorption and accelerates the onset of action. Therefore, it can be applied just before meals, and due to its short effect, the risk of hypoglycemia is reduced.
- Insulin aspart – has similar properties to insulin lispro.
Medium-acting insulins[edit | edit source]
These are cloudy suspensions (mixtures of crystalline and non-crystalline insulin) that are intended only for subcutaneous application.
- Amorphous insulin: a mixture of pork or human insulin with particles of 2 μm with a duration of action of 8-12 hours.
- Zinc-insulin suspension: 330% amorphous insulin and 70% crystalline insulin, the effect lasts differently (from 7 to 24 hours).
- Isophan insulin (NPH insulin or protamine-zinc-insulin): protamine is a mixture of peptides isolated from sperm from river trout. The ratio of protamine molecules to insulin is about 1:6.
- Stabilized insulin mixtures are mixtures of short-acting insulin and insulin isophan. The advantage is a rapid onset and prolonged effect.
Long-acting insulins[edit | edit source]
These insulins are slowly absorbed as they contain large zinc-insulin crystals, so their effect takes slowly but also lasts for a long time (26-28 hours). They are applied subcutaneously, exceptionally intramuscularly. For example, insulin glargine, which has a duration of action of up to 36 hours, is used and must not be mixed with other insulins in one syringe for large crystals.
Schemes[edit | edit source]
Conventional schemes[edit | edit source]
If a certain degree of endogenous insulin secretion is still maintained, the following schemes are used:
- Two-dose scheme: fast and moderate-acting insulin in two daily doses, of which 2/3 of the total daily dose in the morning and 1/3 in the evening.
- Three-dose mode:
- morning: fast insulin + medium-speed insulin,
- before dinner: fast insulin,
- before going to bed: moderate insulin.
Intensified schemes[edit | edit source]
In patients with Type 1 DM, we strive to ensure that the exogenous delivery of insulin best replicates the secretion of insulin from the pancreas of healthy people. These schemes are also used for DM 2nd type with the complicated course.
- Scheme to quickly compensate for diabetes, suitable even for more lymable diabetes: short-acting insulin before the main meals, medium-acting insulin before bedtime.
- Basal-bolus scheme: short-acting insulin before main meals and long-acting insulin in one or two daily doses.
- Schedule of short-acting insulin in at least four daily doses.
- Insulin pump: continuous subcutaneous infusion of fast-acting insulin.
Methods of insulin administration[edit | edit source]
Insulin is given as an injectable solution, most often subcutaneously (rapid insulin can also be given intravenously). Since insulin therapy is permanent, it is necessary to instruct patients accurately and teach them the technique of application so that their diabetes is fully compensated. To apply insulin is used:
Links[edit | edit source]
Related articles[edit | edit source]
- Diabetes mellitus
- Type 1 diabetes mellitus
- Type 2 diabetes mellitus
- Insulin
- Pharmacological possibilities of influencing diabetes
References[edit | edit source]
- ↑ ČEŠKA, Richard. Interna. 1. edition. Praha : Triton, 2010. 855 pp. pp. 233. ISBN 978-80-7387-423-0.
Literature used[edit | edit source]
- LINCOVÁ, Dagmar – FARGHALI, Hassan. Základní a aplikovaná farmakologie. 2. edition. Praha : Galén, 2007. 0 pp. ISBN 978-80-7262-373-0.
- ČEŠKA, Richard. Interna. 1. edition. Praha : Triton, 2010. 855 pp. ISBN 978-80-7387-423-0.
Cathegory:Pharmacology Cathegory:Endocrinology Cathegory:Internal Medicine