Diabetes mellitus, dyslipidemia, obesity
From WikiLectures
Diabetes mellitus (DM)[edit | edit source]
- Type 1 − Selective destruction of β-cells of Pancreas (autoimmunity, LADA) − absolute lack of insulin
- Type 2 − Insulin resistance with a relative deficiency of insulin
- Secondary − Pancreatogenic (surgical removal of pancreas, destruction by inflammation, tumor, injury) − insufficient or no insulin secretion
- Gestational − Hyperglycemia during pregnancy (excessive size of the fetus)
Impaired glucose tolerance (IFG − impaired fasting glucose 5,6 − 6,9 mmol/l, IPG − impaired postprandial glycemia after 2 hours 7,8 − 10,9 mmol/l) DM (2).
- The disease is characterized by hyperglycemia
- Physiological range of glycemia 3,9–5,5 mmol/l
- Determination of glycemia, insulin, C-peptide, glycated hemoglobin (HbA1c), possibly antibodies (anti GAD, ICA) − differential diagnosis DM.
Diagnostic criteria[edit | edit source]
- Fasting glycemia > 7 mmol/l, postprandial glycemia after 2 hours > 11 mmol/l.
Examination of the patient for diabetic complications[edit | edit source]
- Macrovascular (Stroke, acute M.I., ischemic diseases of the lower limbs)
- Microvascular (retinopathy, nephropathy, neuropathy)
Anamnesis, examination[edit | edit source]
- Polydipsia — excessive thirst associated with excessive fluid intake
- Polyuria — excessive urination
- Recurrent bacterial and fungal infections — Urogynecological, respiratory, skin;
- Complications of DM — ophthalmic, neurological, nephrological, vascular, cardiological.
Therapy[edit | edit source]
Dietary measures − basic therapeutic modality:
- Normalization of fasting and postprandial glycemia (Regulation of carbohydrate content in the food and rate of carbohydrate absorption − glycemic index)
- Achieving optimal levels of lipids in blood (TAG, HDL)
- Ensuring sufficient energy supply
- Prevention and treatment of late complications
Diet[edit | edit source]
- 5 − 6 meals per day − second dinner
- Bread units (interchangeable unit)
- 1 BU corresponds to 10 − 12 g of carbohydrates = 2 cubes of sugar (Reducing diabetic diet to 175 g of carbohydrates per day = 16 BU = 32 cubes of sugar)
- Differences in the diet for type 1 and type 2 DM
Pharmacotherapy[edit | edit source]
- Oral antidiabetics
- Influencing the insulin resistance − Biquanides, Thiazolidinediones (glitazones)
- Secretagogues − Derivatives of sulfonylurea, Non-sulfonylureas (glinides)
- Inhibition of digestive enzymes in the GIT (α-glucosidase, lipase)
- Dipeptidyl peptidase-IV inhibitors (gliptins)
- Insulins (human, recombinant, analogues)
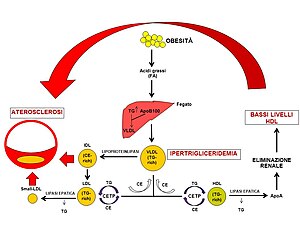
Dyslipidemia[edit | edit source]
- Synonyms − Dyslipoproteinemia, hyperlipidemia, hyperlipoproteinemia
- Lipidogram (lipid profile) − total cholesterol TC, triacylglycerols TAG, low density lipoprotein LDL, high density lipoprotein HDL, apolipoprotein B (apo B), apolipoprotein AI (apo AI)
- Dyslipidemia is characterized by an altered Cholesterol level and/or triacylglycerides and/or HDL cholesterol
- Atherogenic lipid phenotype − TAG, jLDLsd, J.HDL.
Division[edit | edit source]
- Etiology
- Primary − Genetic and lifestyle factors (composition and amount of food, smoking, alcohol, physical activity and body weight)
- Secondary − Other diseases are involved in the development of dyslipidemia
From the clinical and therapeutic perspective, dyslipidemia is divided into three groups:
- Isolated hypercholesterolemia
- Increased total Cholesterol (TC), mostly in the LDL-cholesterol fraction (LDL−C), with a normal concentration of triacylglycerides (TAG);
- Isolated hypertriacylglycerolemia
- Increased TAG in combination with a normal cholesterol concentration (TC);
- Combined hyperlipidemia
- Simultaneously increased levels of both TC and TAG.
Therapy[edit | edit source]
Lifestyle changes
- Restricted diet, no consumption of alcohol, smoking, physical activity
Diet
- Limiting intake of fat to 60 g/day, cholesterol intake 300 mg/day (egg yolk contains 250 mg), consumption of fiber 30 g/day − 500 g of fruits and vegetables, processed foods.
Pharmacotherapy
- Statins (atorvastatin, simvastatin, fluvastatin, rosuvastatin)
- Fibrates (fenofibrate)
- Ezetimibe
- Bile acid resins (Questran)
- Combination of medications (simvastatin/ezetimibe)
Conclusion[edit | edit source]
Aiming to reach optimal levels of lipids, weight, and blood pressure to reduce the risk for cardiovascular diseases and mortality.
Obesity[edit | edit source]
- Excessive storage of fat in the organism
- Classification according to quantity (BMI) and quality (android type, gynoid type)
- Physiologic amount of fat in women is 25−30 % and in men 20−25 %
- BMI = weight (kg)/height (m)2.
Classification of body weight according to BMI[edit | edit source]
Anthropometry
- Waist circumference − site of measurement: visible waist, respectively at the level of iliac crest and last rib
- Physiologic value − men up to 94 cm, women up to 80 cm
- Measurement of skin folds − bicipital, tricipital, subscapular, suprailiac
- Bioelectrical impedance analysis for percentage of fat.
Therapy[edit | edit source]
- Aiming to reduce weight by 5−10 % and maintaining this weight
- Significant reduction of risk for DM, hypertension, and cancer
- Reduction of risk for complications of obesity − diseases of the musculoskeletal system, dyspnea and sleep apnea syndrome.
Diet therapy
- Restricted diet − regular meals, 5 − 6 times per day, regulated amount of proteins, less fat and sugar, limited amount of table salt (605 − 1770 kcal/day)
- Pharmacotherapy − Anti-obesity drugs: sibutramin, orlistat, rimonabant
- Physical activity − Exercise test (ergometry)
Metabolic syndrome[edit | edit source]
Raven syndrome, syndrome X
- According to IDF 2005: waist M 94 cm and more, F 80 cm and more, increased TAG, arterial hypertension, DM or impaired glucose tolerance
- Significant impact on quality of life, increased morbidity (complications of DM, dyslipidemia...), mortality (CVD)
Anamnesis[edit | edit source]
- Family history: DM, endocrinopathies, CVD, Metabolic syndrome
- Personal history: co-morbidities − DM + complications, CVD, nephropathy, endocrinopathies, infections
- Gynecological history: deliveries, fetal weight (more than 4 kg), abortions
- Addictions: smoking, alcohol consumption, drugs
- Pharmacological history: corticoids, oral contraceptives, hormone replacement therapy, thyroid hormones, psychiatric drugs, oral antidiabetics, insulin
Conclusion[edit | edit source]
- Complex approach − psychology, psychopathology, patient habits, background
- Adjustment of lifestyle − physical activity
- Diet therapy − planning of meals
Links[edit | edit source]
Original text is from Wikiskripta – https://www.wikiskripta.eu/index.php?curid=36984
Related articles[edit | edit source]
Source[edit | edit source]
- DUŠEJOVSKÁ, M.. Diabetes mellitus, dyslipidemie, obezita [online]. [cit. 2012-03-11]. <https://el.lf1.cuni.cz/att00082/>.
- KAREN, Igor – SVAČINA, Štěpán. Diabetes mellitus v primární péči. 2. edition. Prague. 2014. ISBN 978-80-904899-8-1.
- GANONG, William F. Přehled lékařské fysiologie. 1. edition. Jinočany : H & H, 1995. 681 pp. ISBN 80-85787-36-9.
- SVAČINA, Štěpán. Poruchy metabolismu a výživy. 1. edition. Praha : Galén, 2010. 505 pp. ISBN 978-80-7262-676-2.