Cancer of the bladder
From WikiLectures
This article has been translated from WikiSkripta; ready for the editor's review.
Currently, they make up more than 2 % of newly diagnosed malignant tumors.
Epidemiology[edit | edit source]
- Morbidity is still increasing, mortality is decreasing, it affects 3x more often men,
- high incidence – in SW Europe, low in India and Japan,
- the main occurrence is between 50 and 70 years.
Etiology[edit | edit source]
- The main risk factor is smoking (mainly smoking black tobacco),
- exposure to some industrial pollutants – aromatic amines (benzidine, 2-naphthylamine, ...),
- chronic infection, in endemic areas – schistosomiasis (does mainly squamous cell ca).
Clinical Manifestations[edit | edit source]
- Hematuria and polakisuria,
- increased bladder irritability is indicative of throat involvement, hydronephrosis and secondary pyelonephritis may occur in the case of involvement in the area of the mouth of the ureters,
- sometimes it can be completely asymptomatic,
- general symptoms (loss of appetite, weight loss, anemia) - they only occur in very advanced tumors.
Diagnostics[edit | edit source]
- Cystoscopy,
- endoscopic biopsy, possibly transurethral resection → this is absolutely necessary to determine the stage.
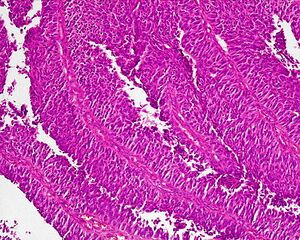
Histopathology[edit | edit source]
- 97 % are carcinomas of the urothelium, rarely adenocarcinomas and undifferentiated carcinoma, squamous cell is endemic (schistosomiasis),
- macro - different appearance - papillary, infiltrating, about ¼ arise multicentrically (this is the cause of frequent recurrences),
- may begin as ca in situ and then progress to a papillary or an infiltrating form,
- initially the tumor grows in the mucosa, then early on it grows into the submucosa, muscle and surrounding fat, it metastasizes to the pelvic nodes, later the para-aortic nodes, rarely hematogenously.
Treatment[edit | edit source]
The method of therapy depends on a careful evaluation of the histology, the degree of invasion, the extent of the disease.
Surgical treatment[edit | edit source]
- Non-invasive tumors can be treated by transurethral resection (TUR) - it is a relatively less damaging procedure, it does not affect the function of the bladder,
- to treat surface structures - coagulation or laser vaporization,
- but relapse often occurs within 1 year, therefore the five-year survival rate does not exceed 80 %,
- that is why it is recommended to add adjuvant intravesical CHT, intravesical application of IFN, BCG vaccine, adriamycin, irradiation,
- if the tumor grows into the muscle - partial cystectomy,
- the rationality of this procedure is questioned due to the multifocal origin of urothelial tu,
- in addition, there is a risk of implantation meta, that is why it is practically not carried out today,
- for more extensive tumors - radical cystectomy with lymphadenectomy, in men with prostatectomy in women with hysterectomy, adnexectomy,
- it is a very demanding performance and its indications must be carefully considered.
Radiotherapy[edit | edit source]
- Most often as external irradiation, it is not used as a separate treatment, for numerous NU,
- even as a neoadjuvant, a significant effect was not confirmed,
- radiochemotherapy (RCHT) might have a good effect so far, but this is not supported by studies,
- is, however, irreplaceable as palliation (meta analgesia to the skeleton, suppression of hemorrhagic complications).
Chemotherapy[edit | edit source]
- Administered either locally or systemically,
- local – for diffuse ca in situ, for superficial tumors after TUR and for papillary ones (the most advantageous nowadays is mitomycin C, which is practically not absorbed from the bladder and does not pose a threat of toxicity),
- systemic – the main palliative treatment of advanced forms, the tumor responds to a number of cytostatics,
- corresponds most to – Pt derivatives, anthracyclines, ifosfamide,
- adjuvant CHT – very useful especially in cases of involvement of nodes,
- neoadjuvance – has many disadvantages, it is not done as standard.
Photodynamic therapy[edit | edit source]
- It can be effective in ca in situ and in papillary ca.
Immunotherapy[edit | edit source]
- Mainly in the form of local application BCG.
Prognosis[edit | edit source]
- For non-invasive, 5-year survival is 75-80 %.
Links[edit | edit source]
Related Articles[edit | edit source]
External links[edit | edit source]
Source[edit | edit source]
- BENEŠ, Jiří. Study materials [online]. ©2010. [cit. 2010-06-16]. <http://jirben.wz.cz>.