Biochemical analysers
Biochemical analyzers became a part of clinical laboratory practice in the 1970s as a continuation of the process of mechanization of laboratory activities. The elements of mechanization were the use of piston pipettes and piston-valve dispensers to measure biological material and dispense reagents, pouring or flow-through cuvettes for photometers, and varying degrees of mathematical processing of the measured signal (absorbance) of calibrators and samples with the printing of the resulting concentration of the measured analyte. Biochemical analyzers became a part of clinical laboratory practice in the 1970s as a continuation of the process of mechanization of laboratory activities. The elements of mechanization included the use of piston pipettes and piston-valve dispensers for measuring biological material and dispensing reagents, pouring or flow-through cuvettes for photometers, and varying degrees of mathematical processing of the measured signal (absorbance) of calibrators and samples with printing of the resulting concentration of the measured analyte. Currently, in addition to the biochemical analysers used in the routine operation of a clinical biochemistry laboratory, portable benchtop analysers of various types are also used. They are used for rapid determinations in small laboratory operations, in the offices of general practitioners, specialists, or at the patient's bedside. The latter application is represented by the very extensive, diverse and still developing POCT (Point of Care Testing) system. A specific feature of POCT analysers is their simple operation, highly developed self-diagnostic system with minimal requirement for calibration, inspection and maintenance by untrained laboratory personnel. The usual solution is the so-called cartridge system, where the inserted cartridge contains all necessary reagents, calibration and control materials, or other necessary disposable components such as measuring electrodes. The POCT analysers are subject to the so-called supervision of laboratory staff. This is simplified by their on-line connection to hospital networks, which allows remote management, monitoring of their function, evaluation of automatically performed control analyses and transfer of measured data to laboratory and hospital information systems. The price for fast availability and easy operation is significantly higher financial costs compared to conventional laboratory testing.
Automatic analyzers[edit | edit source]
The automated analysers were able, without operator intervention, to perform the individual steps of biochemical analysis according to a pre-programmed algorithm. This involved the transport of the analytical sample, pipetting, reagent dosing, mixing, incubation, measurement of absorbance changes, calculation of concentration using calibration standards, display and printing of the biochemical analysis result, or its transfer in the electronic form to the laboratory information system. In addition to the basic spectrophotometric principle of measuring absorbance changes, the analysers use many other measurement principles, such as immunoturbidimetry, chemiluminescence, enzyme-linked immunosorbent assay on microparticles, fluorescence polarisation immunoassay, etc. A standard component of biochemical automatic analyzers is a module with ion-selective electrodes (ISE) for the determination of Na+, K+ and Cl-.
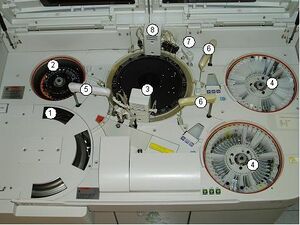
The main components of an automatic analyzer:
- transport system transporting samples in racks to the serum pipettor,
- rotor in the refrigerated compartment for calibrators, controls and statim samples,
- rotor with reaction cuvettes stored in a water bath tempered to 37 °C,
- reagents (R1, R2) in bar-coded containers; the cooled compartment is closed with a lid during operation,
- serum pipettor,
- reagent pipettor - dispenser,
- rotary stirrer,
- reaction cell washing station.
Current automated biochemical analysers belong to the generation of selective random access analysers that allow a free choice of dozens of methods for a single sample. The hourly performance of different types of analysers varies. Values range from 100 to several thousand analyses per hour. Important for the performance is the so-called analyzer clock, i.e. the time in seconds after which the reaction cuvette is periodically paused to allow the next sample to be pipetted. At a clock rate of 4 s, this is 15 tests per minute and 900 tests per hour. A regular feature of the analysers is the possibility to preferentially perform analyses in a so-called statim sample. The time response to these samples is calculated in minutes. The described tasks are solved differently by different manufacturers, sometimes uniquely, using patented procedures. Aware of some simplification, in the following we limit ourselves to describing an example of a standard solution.
Analyser components[edit | edit source]
The transport system' transports analytical samples from the analyzer inlet to the pipettor work area and, after pipetting, to the analyzer output. It is most often provided by moving the sample racks in a linear or rotary motion. A laser barcode reader is located at the input of the analyser. The barcode uniquely identifies the sample for linking to patient data in the laboratory information system and also informs the analyser of the type of material being analysed (serum, plasma, urine, liquor, etc.).
The Pipetor' provides pipetting of the sample into the reaction cuvette. The pipetting needle is made of inert material and is equipped with a level sensor (conductivity, capacitive, radio frequency system) that stops the vertical movement of the pipettor when the needle contacts the sample surface so that the sample is drawn in just below the surface. Pipetting volumes range from 2-20 μl. To prevent contamination, transfer (carry over), the pipetting needle is washed externally and internally in a washing station when moving to the next sample. Where very low concentrations are measured, the analyte to be measured is present over a wide concentration range and there is a high risk of contamination with false positive results, the analysers use pipette tips that are automatically changed when moving to the next sample.
Reagent dispensers' work on the same principle, including level sensors and a washing station to prevent cross-contamination of reagents. The volumes dispensed are programmable in a range corresponding to the volume of the reaction cuvette, e.g. 20-300 μl. Precise sample volume measurement and reagent dispensing is provided by piston dispensers that are connected to the pipettor end tubing. Volume changes during the movement of the Teflon pistons are transferred to the pipettor end needles.
Reaction cuvettes differ according to the material used, shape, volume and method of use, either as disposable, which are disposed of in the waste after use, or reusable after automatic washing. The basic requirement is the UV permeability of the cuvette material, which is met by synthetic materials and quartz glass. Gradual miniaturisation is leading to cuvettes with a content of less than 100 μl.
Incubation bath is the environment in which the reaction cuvettes are placed. The incubation temperature, which is particularly important for the determination of the catalytic concentration of enzymes, is maintained at 37 °C with an accuracy of ± 0,1 °C. A homogeneous temperature environment is provided by circulating water, oil or air in the incubation bath.
Light source' - monochromator' - absorption medium' - detector. A halogen or xenon lamp is usually used as a light source; the light beam of a continuous spectrum, after passing through the absorption medium (cuvette), is decomposed by the monochromator (optical grid) into beams of defined wavelength (monochromatic radiation), which fall on the detector, usually a diode array (diode array). Changes in the absorbance of the reaction mixture in the cuvette are monitored (recorded) each time the cuvette passes through the beam of the optical system.
Reagents'. Automatic biochemical analysers allow the use of two reagents per method (two-step methods) as standard, but 3 to 4 reagents can also be used. Reagents can be in liquid form (liquid-ready to use), for less stable reagents they are prepared by dissolving a powder or tablet form before being loaded into the analyser. They are stored in the analyser in refrigerated areas to increase their stability and reduce evaporation. The reagent containers are usually labelled with a barcode which is registered by the analyser and thus does not depend on their position in the reagent compartment. Before dispensing the reagent into the cuvette, the appropriate container is set to the pipetting position of the appropriate dispenser.
The stirrer provides mixing of the reaction mixture in the cuvette, for example by rotary movement of the stirrer blade briefly immersed in the reaction cuvette, or by vibration, ultrasound or air bubbling.
The washing station extracts the reaction mixture at the end of the measurement and prepares the cuvette for further use by repeated rinsing with water and final drying.
Parameter-definition methods'. Each method has defined parameters: method of measurement (end point, kinetic), wavelengths, the volume of sample pipetted and reagents dispensed, determination of measurement points for concentration calculation, measurement of absorbance rise or fall, limits for repeating the analysis with a larger or smaller sample volume at too high or too low concentration.
Results display and transfer'. The results of the analyses are continuously displayed on the analyzer screen, printed on the analyzer printer, transferred to the laboratory information system via on-line connection, or further in the electronic form to the hospital information system in the patient's records.
The course of the reaction'. Changes in the absorbance of the reaction mixture in the cuvette are continuously monitored and graphically recorded (reaction monitor). The graphical recording throughout the incubation period is particularly important in the determination of catalytic enzyme concentrations, where it allows the detection of substrate depletion at high enzyme activity, non-linear or otherwise altered reaction progress.
Error messages, self-diagnosis'. All activities and functions of the analyzer are programmed in the software of the control computer. The movement of the moving parts of the analyzer is mostly provided by precision stepper motors. The correct function of the moving parts is continuously monitored by special sensors that control the end position and the time required to reach it. If the set positions and time limits are not met, the analyzer stops with an associated error message. The water in the analyser is driven by pumps and vacuum extraction, which is controlled by magnetic valves.
Current electronically controlled automated biochemical analysers often have highly sophisticated software. Statistical evaluation of control analyses in numerical and clear graphical form and internal quality control tools allowing selection and combination of Westgard rules are common. Another software application is, for example, the so-called reflex mode, which allows for the automatic execution of additional analyses when a pathological value of the ordered test is present.
A characteristic feature of the development of automated analytical systems in recent years has been the construction of hybrid systems combining analysers using different spectrophotometric principles with immunochemical (homogeneous and heterogeneous) immunoassays. The two types of analyzers were connected by a different conveyor system to transport the biological samples and the measured data were concentrated in a single result sheet.
Nowadays, manufacturers of automated laboratory systems have focused on the development and production of automated and robotic lines that cover the pre-analytical and post-analytical phases of laboratory processes. So-called total laboratory automation has become realistic and relatively accessible.
Preanalytical process in the laboratory consists of:
- receipt and identification of the biological sample,
- centrifugation,
- "declogging",
- aliquoting,
- labeling of aliquots with barcode labels,
- sorting of primary and secondary samples (aliquots) - sorting,
- for on-line connections, direct entry into the conveyor system of the analytical section.
Post-analytic process means:
- validation of analytical results,
- electronic transfer to the laboratory information system,
- archiving of primary or aliquot samples.