Scrotum and Coverings of Testis
Scrotum
It is cutaneous sac, consisting of 2 layers: the heavily pigmented skin and the dartos fascia. The Dartos fascia a fatty-free fascial layer including smooth muscle fibers, is responsible for the pigmentation. When cold, the dartos muscle fibers contract the skin and make the scrotum wrinkle, reducing the surface area of the scrotum and assisting the cremaster muscles in holding the testes closer to the body, thus reducing heat loss. The scrotum is divided internally by a continuation of the dartos fascia in the scrotal septum, into right and left compartments. The septum is demarcated externally by the scrotal raphe.
Vasculature & Innervation
- Arterial Supply:
- posterior scrotal branches of the perineal artery;
- anterior scrotal branches of the deep external pudendal artery
- cremasteric artery (branch from inferior epigastric artery).
- Venous drainage: by the venae comitantes of the arteries.
- Lymphatic drainage: into the superficial inguinal lymph nodes.
- Innervation:
- genital branch of genitofemoral nerve (suppies anterolateral surface);
- anterior scrotal nerves from ilioinguinal nerve (supply anterior surface);
- posterior scrotal nerves from perineal nerve from pudendal nerve (supply posterior surface);
- perineal branches of the posterior femoral cutaneous nerve (supply inferior surface).
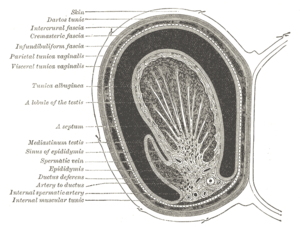
Coverings of testis
Numbering from deep to superficial:
- Tunica vaginalis (visceral layer)/epiorchium
- Tunica vaginalis (parietal layer)/periorcium (from peritoneum)
- Internal spermatic fascia (from tranversalis fascia)
- Cremaster muscle and its fascia (from internal oblique muscle)
- External spermatic fascia (from external oblique muscle)
- Dartos fascia
- Skin
Descent of testis
The testes descent at the end of the fetal development, under guidance of the gubernaculum testis, into the scrotum. They are originally intra-peritoneally, and thus after descent, their tunica vaginalis is a remnant of infolded peritoneum. When they exit the abdominal cavity, they ensure the decrease of 2–5 °C in temperature, required for proper spermatogenesis. The higher temperature in the abdominal cavity only interferes with spermatogenesis and not with hormone production. At around the 8th month, the testes reach the superficial inguinal ring and lie in the scrotum at the beginning of the 9th month. As it proceeds downwards, along posterior wall of the peritoneum, inside the processus vaginalis peritonei (peritoneal evagination), which in turn forms a cavity around the testis (made of the 2 layers, parietal and visceral, of tunica vaginalis. The connection with the abdominal cavity is therefore then, normally, obliterated.
Links
Related articles
Bibliography
- MOORE, Keith L – DALLEY, Arthur F. Clinically Oriented Anatomy. 5. edition. Lippincott Williams & Wilkins, 2005. ISBN 0781736390.