Epidural Anaesthesia
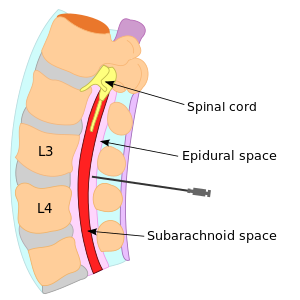
Epidural anesthesia is method based on application of local anesthetic into epidural space. It is a type of local neuraxial blockade.
Anatomy[edit | edit source]
Epidural space (= extradural space) is localized in spine canal between ligamenta flava and dura mater. Contains loose connective tissue. The pressure in epidural space is lower than atmospherical pressure (will be useful). Epidural space is 3–5 mm wide and has no horizontal borders – epidural anesthesia works, where is applied.
Performance[edit | edit source]
Epidural anesthesia can be performed anywhere in entire length of the spine. Patient lies on his side, we start with disinfection of skin and application of small dose of local anesthetic into skin. After local anesthetic starts work, we can insert Tuohy needle (it has slightly curved end, is used for epidural catheter insertion). It is difficult to recognize epidural space, there are two techniques of insertion[1]:
- Loss of resistance technique – the needle is connected with special syringe filled by saline solution, while we are inserting the needle, we are continuously pushing on the piston of the syringe, there is a loss of resistance.
- Hanging drop technique – there is a drop of saline solution hanging in the external end of needle, when we reach the epidural space, the drop is sucked into the needle (there is lower pressure in epidural space!).
Then we can insert catheter and remove the needle. There is possibility of single shot application.[1]
Effects[edit | edit source]
- local anesthesia
- motor blockade
- sympathetic blockade
Range (number of dermatomes) of epidural anesthesia is done by it's localization and amount of local anesthetic (1,5–2 ml for 1 dermatome). Intensity of epidural is done by concentration of local anesthetic:
- low concentration – local anesthesia (sensitive fibers – are on the surface),
- higher concentration – motor block (motor fibers – are deep inside).[1]
Indications and Types[edit | edit source]
General indications are:
- perioperative analgesia,
- postoperative analgesia,
- chronic pain managment.[2]
Types[edit | edit source]
- Lumbar epidural – (L2–5) lower extremity operation, inguinal hernias, cesarean section and childbirth.[2]
- Thoracic epidural – lower thoracic level (Th7–12) – laparotomy, cholecystectomy, or upper thoracic levels (Th1–7) for postoperative analgesia of thoracotomy, sternotomy. Performed only with catheter.[2]
- Cervical epidural – C6–C7 or C7–Th1 level, carotid endarterectomy, strumectomy and hand surgery.[2]
Complications[edit | edit source]
Complications are more frequent than in spinal anaesthesia. Higher risk of complications is in pregnant women because of swelling of tissues caused by progesterone, epidural space is thinner.
- postpuncture headache – if the subarachnoid space and dura mater is violated,
- bleeding,
- infection,
- spinal haematoma formation is very dangerous and needs acute surgery,
- anaphylactic or toxic reaction to the anaesthetic.
Links[edit | edit source]
Related Articles[edit | edit source]
References[edit | edit source]
- ↑ a b c MÁLEK, J – DVOŘÁK, A, et al. Základy anesteziologie. 1. edition. Praha. 2009.
- ↑ a b c d MICHÁLEK, Pavel. Regionální anestezie [lecture for subject Anesteziologie, specialization General Medicine, 1. LF UK Charles University in Prague]. Prague. 2012. Avaliable from <http://www.karim-vfn.cz/userfiles/download/003-regionalnianestezie-1317888703.pdf>.