Corpus Luteum
|
This article was marked by its author as Under construction, but the last edit is older than 30 days. If you want to edit this page, please try to contact its author first (you fill find him in the history). Watch the discussion as well. If the author will not continue in work, remove the template Last update: Monday, 08 Dec 2014 at 6.44 pm. |
Corpus Luteum[edit | edit source]
The Corpus Luteum (Latin: "Yellow Body") is a temporary endocrine structure in mammals, responsible for production of progesterone, estradoil and inhibin A.
Development and Structure[edit | edit source]
The Corpus Luteum is formed in the ovary. It arises from Granulosa cells that remain in the wall of the ruptured follicle, after the oocyte has been extruded into the Uterine tube. Granulosa cells, together with the cells of Theca Interna, are vascularized by surrounding vessels.
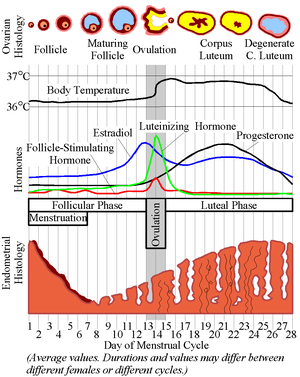
Under the Influence of LH (Luteinizing Hormone), produced by the Adenohypophisis, Granulosa cells increase greatly in size (20-35μm in diameter) without dividing, and eventually comprise about 80% of the parenchyma of the Corpus Luteum. They are then called granulosa lutein cells, and have lost many features of protein-secreting cells. They instead expand their role in aromatase conversion of androstenedione into estradiol.
The Theca interna gives rise to the theca lutein cells, contributing the other component of the corpus luteum. These cells are less than half the size of granulosa lutein cells, and often stain darker, with cytoplasmic structures of steroid-syntesising cells.
The Corpus Luteum is relatively large, during pregnancy (Corpus Luteum graviditatis), it can be one third to one half of the size of the ovary.
Once the Corpus Luteum regresses, it forms the Corpus albicans.
Function[edit | edit source]
The Lutean cells of the Corpus luteum secrete progesterone and estrogens. These hormones cause the uterine mucosa to enter the secretory (progestational) stage in preparation for implantation of the embryo.
Estrogen produced the by corpus luteum inhibits the release of Follice stimulating hormone (FSH) from the pituitary, preventing follice formation and multiple ovulation. If fertilization does not occur, the corpus luteum reaches it's maximum developlment at aprox. 9 days after ovulation. With no further LH stimulation, both major cell types undergo apoptosis, while the tissue regresses. This results in decreased progesterone production and menstruation occurs. The inhibition of FSH also ends, and a new group of follicles are stimulated to grow, marking the beggining of another menstrual cycle. The Corpus luteum that lasts for only a part of a menstrual cycle is the corpus luteem of menstruation. It's remntants are phagocytosed by macrophages, after which fibroblasts invade the are and produce a scar of dense connective tissue, the corpus albicans. (Latin: White body)
However, if pregnancy does occur, the corpus luteum needs to be preserved in order for the embryo to survive (otherwise, menstruation would occur). To prevent the drop is circulation progesterone, the trophoblast of the embryo produces a glycoprotein hormove, human chorionic gonadotropin, the action of which is similar to LH. By this mechanism the corpus luteum is preserved and stimulated. The corpus Luteum of pregnancy becomes very large and is maintained by HCG for 4 to 5 months, until the placenta itself produces adequate progesterone and estrogen levels for maintaing the unterine mucosa.
Bibliography[edit | edit source]
SADLER, T. W., et al. Langman's Medical Embryology, 11. Edition. Lippincott Williams & Wilkins, 2009. ISBN 978-0-7817-9069-7
MESCHER, Anthony L., Junqueira's Basic Histology, 12. Edition. Mc Graw Hill, 2010. ISBN 978-0-07-127190-5.